You are here
INCLUDE Project/Down Syndrome Research Plan
The NIH INCLUDE/Down Syndrome (DS) Research Plan will help guide and coordinate NIH-wide research activities for the next five years. Review the full NIH INCLUDE/DS Research Plan on this page or download the printable version. The appendices for the plan are only available as PDFs at this time.
On this page
Executive Summary Introduction Portfolio Analysis Goals & Objectives Conclusion Appendices
Executive Summary
Since the last National Institutes of Health (NIH) Research Plan on Down Syndrome was published in 2014, the research community has made a great deal of progress in understanding many of the co-occurring conditions that impact the lives, health, and well-being of people with Down syndrome (DS). Many NIH-funded studies have addressed aspects of the prior research plans and contributed to improved knowledge of the pathophysiology, treatment, and management of DS. A number of publications demonstrate these advances.
In late fiscal year 2018, the NIH-wide INvestigation of Co-occurring conditions across the Lifespan to Understand Down syndromE (INCLUDE) Project launched to better understand co-occurring conditions that are prominent in those with DS, as well as in the general population. Congressional report language provided several directives to guide DS research and its evolution through the INCLUDE initiative. Although the INCLUDE Project has already stimulated research within its three main components of basic science, cohort building, and clinical trials for those with DS, the value of this investment is just starting to be realized. Certainly, the infusion of dedicated funding for DS research through the INCLUDE Project has catalyzed new avenues of research through a suite of new funding opportunity announcements. The commitment of funds also expands NIH’s ability to support the next generation of DS researchers and trainees and to enhance career development through the INCLUDE Project and other mechanisms. The INCLUDE Project also brings NIH institutes, centers, and offices into the field that have not traditionally supported research in DS by systematically addressing co-occurring health conditions. These coordinated research efforts are focused on developing more treatments for those with DS across the lifespan and on supporting clinical trials to rigorously demonstrate treatment efficacy.
The Portfolio Analysis section of this research plan offers a broad overview of NIH-funded projects and summaries of some of the key DS research findings, identified from the projects’ nearly 600 publications over the last 7 years, ending in December 2020 (see Appendix G: Bibliography). This plan also incorporates feedback from many groups that represent the DS community, including: investigators; members of advocacy groups and professional organizations, such as those comprising the DS Consortium (see Appendix A: NIH-Led DS Groups; parents and other family members; and individuals with DS. Appendix B: Input into Development of the Revised Plan outlines the process used to develop this research plan. Summaries of the NIH-supported meetings, workshops, and symposia that focused on DS are available in Appendix D: DS-Research Related Meetings Since 2014.
With this broad input and new opportunities in DS research in mind, the plan reflects five broad themes organized into goals and objectives for NIH DS research:
- Basic Research
- Cohort Development/Epidemiology
- Clinical Research/Co-occurring Conditions
- Living and Aging with DS/Services Research
- Research Infrastructure and Tools
A “Program Portrait” for each section highlights a particular project or initiative that has made significant progress toward addressing that objective. Several new objectives emphasize the importance of increasing inclusion of those with intellectual disabilities in research that affects them, as reflected in the Increase Inclusion of People with DS in Research section within Theme D: Living and Aging with DS/Services Research. The need for greater diversity among both investigators studying DS and the DS populations they study is also a focus, mirroring calls for equality and representation in biomedical research in the United States.
The plan’s conclusion summarizes recent and future developments that will inform emerging research opportunities in the years to come. For example, the recent recognition that those with DS have altered immune responses to viral infections, such as SARS-CoV-2, adds an urgency to the research activities described in this plan.
This research plan offers a roadmap for DS-related research that can only be accomplished by partnerships among researchers, clinicians, family members, other stakeholders, and most importantly, those with DS, who have much to teach the world.
Introduction
This plan builds upon earlier National Institutes of Health (NIH) research plans on Down syndrome (DS), published in 2007 and 2014, and on the 2018 research plan for the INvestigation of Co-occurring conditions across the Lifespan to Understand Down syndromE (INCLUDE) Project. The previous NIH DS research plans have been integrated with the INCLUDE Project’s goals and with extensive public input, including responses to two Requests for Information issued to the general community, to create this comprehensive NIH INCLUDE Down Syndrome Research Plan. A description of the full development process is available in Appendix B: Input into Development of the Revised Plan.
This plan provides the research, clinical, and DS communities with NIH’s strategy to support high-quality, focused research addressing critical health and quality-of-life needs for individuals with DS and their families. Moreover, this plan incorporates more inclusive language to describe people with DS and their families. For example, the plan refers to “people with DS” rather than “patients,” and uses “co-occurring conditions” rather than “comorbidities.” In keeping with NIH policy on inclusion in research across the lifespan, this plan demonstrates that research efforts should include people with DS of diverse ages, socioeconomic levels, and racial and ethnic backgrounds.
People with DS may have a higher incidence of certain chronic, health- or life-threatening conditions, but are highly protected from other conditions. This health challenge generated the initial interest of Congress, which directed NIH to develop what later became the INCLUDE Project. The breadth of co-occurring conditions covered by the INCLUDE Project garnered involvement of many of NIH’s institutes, centers, and offices (ICOs), each contributing its expertise to the investigation of those conditions (see Appendix A: NIH-Led DS Groups). The increases in funding provided by the INCLUDE Project have catalyzed new investments in DS research across NIH (see Figure 1 and Table 1). Not only will research into these co-occurring conditions improve the care and health of people with DS, but it could also lead to a deeper understanding of these conditions in people who do not have DS, ultimately leading to treatments for the general population. Please note that although the appendices and other sections of this document include 2021 information, the portfolio analysis only includes information through December 2020.
Figure 1: NIH Down Syndrome Research Funding 2011 to 2020
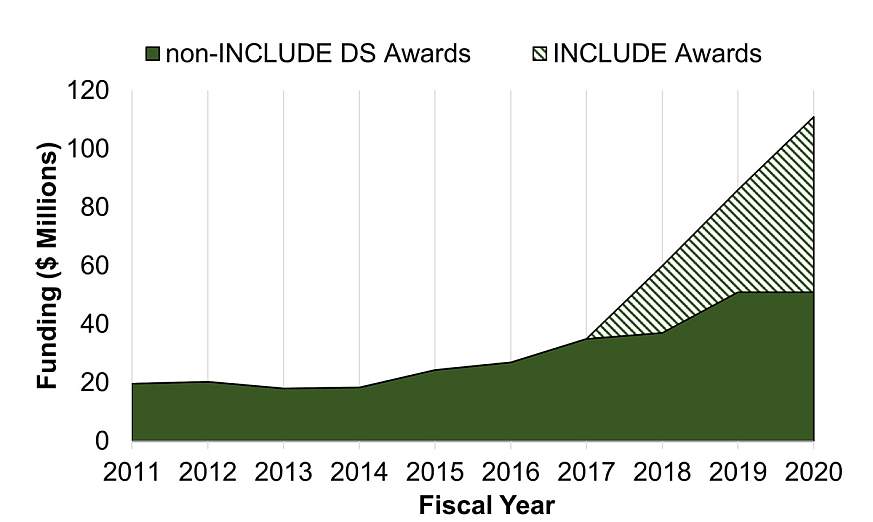
Table 1: NIH Down Syndrome Research Funding, Fiscal Year 2011 to 2020
(all amounts in millions of U.S. Dollars)
|
Fiscal Year |
Non-INCLUDE DS |
INCLUDE |
Total |
|---|---|---|---|
|
2011 |
19.7 |
NA |
19.7 |
|
2012 |
20.3 |
NA |
20.3 |
|
2013 |
18 |
NA |
18 |
|
2014 |
18.3 |
NA |
18.3 |
|
2015 |
24.3 |
NA |
24.3 |
|
2016 |
26.9 |
NA |
26.9 |
|
2017 |
35 |
NA |
35 |
|
2018 |
37 |
23 |
60 |
|
2019 |
51 |
35 |
86 |
|
2020 |
51 |
60 |
111 |
Research on co-occurring conditions of people with DS does not happen in a vacuum; it builds on generations of basic research discoveries to develop an understanding of the genetic and physiological underpinnings of DS and the wide variation in the conditions experienced by individuals with DS. NIH’s goal is to prevent these conditions from limiting the capacity of people with DS to lead healthy and optimal lives.
The goals and objectives of the NIH INCLUDE Down Syndrome Research Plan represent a hybrid of two previous DS plans:
- Down Syndrome Directions: The NIH Research Plan on Down Syndrome, published in 2014, which was organized into shorter term and longer term objectives with the following themes: Pathophysiology of DS and Disease Progression; DS-Related Conditions: Screening, Diagnosis, and Functional Measures; Treatment and Management; DS and Aging; and Research Infrastructure
- The INCLUDE Project 2018 Research Plan, which was organized into three components: conduct targeted, high-risk/high-reward, basic science studies on chromosome 21 and DS; assemble a large cohort of individuals with DS across the lifespan; and include individuals with DS in existing and future clinical trials
For this research plan, goals and objectives are organized around five broad themes:
- Basic Research
- Cohort Development/Epidemiology
- Clinical Research/Co-occurring Conditions
- Living and Aging with DS/Services Research
- Research Infrastructure and Tools
Each goal includes groups of objectives, as well as a “Program Portrait” highlighting a specific research project that addresses the theme.
Portfolio Analysis
To analyze the progress made in DS research since 2014, NIH undertook a systematic review of articles from NIH-funded projects published between January 2014 to December 2020, inclusive. A total of 722 publications were identified using the Medical Subject Heading-extracted term “Down syndrome” and the NIH portfolio analysis tool, iSearch. Please note that although the appendices and other sections of this document include 2021 information, the portfolio analysis only includes information through December 2020.
Four subject matter experts (SMEs) curated publications for relevance to DS, the category addressed from the 2014 Research Plan, and status as a critical discovery or accomplishment in the field. At least two SMEs coded each article, and coding discrepancies were resolved by consultation involving all four SMEs. Publications excluded as not relevant to DS were those related to a gene or protein on chromosome 21 with “Down syndrome” in its name, those representing a small case study, or those with minimal mention of DS.
A total of 592 publications were included in the analysis, representing about 82 percent of the original search results. Four additional articles were added that either referenced NIH-related workshops or resources, or that were review articles supported in part by NIH awards, but not identified through the original iSearch portfolio review process. The final total of 596 publications represents a 75-percent increase over the 340 publications cited in the 2014 DS Research Plan.
Articles were assigned to one of the five themes from the 2014 DS Research Plan (see Figure 2), with about 80 percent to 95 percent concurrence between two assigned curators; resolution of discrepancies was made by one curator for consistency. There were notable increases in the number of publications in the categories of “DS-Related Conditions,” “DS and Aging,” and to a lesser extent, “Treatment and Management.” (See Appendix G: Bibliography for the full list of publications grouped by categories from the 2014 DS Research Plan.)
Figure 2: DS-Research Related Publications, 2014 to 2020,
by 2014 DS Research Plan Theme Area
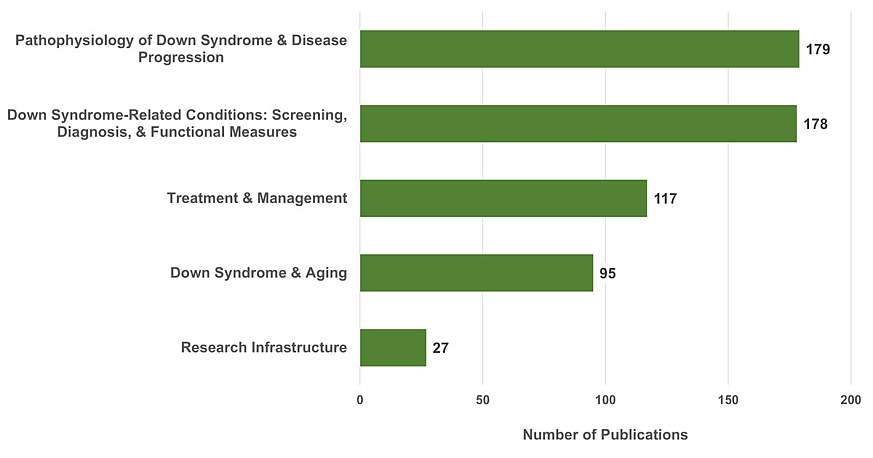
Given the short duration since the start of the INCLUDE Project (slightly more than 2 years between the issuance of the first awards and the portfolio analysis), the contribution from INCLUDE-funded projects cannot yet be quantified. Most projects have had not had adequate time to generate data that would support publications.
Highlights from the DS-related research accomplishments since 2014 within each theme are as follows.
Pathophysiology of DS and Disease Progression
Our understanding of the basic mechanisms that underlie co-occurring conditions described in people with DS continues to evolve. Although the precise underpinnings are not well understood, the general molecular and genetic bases of DS are presumed to result from altered gene expression stemming from an extra copy of chromosome 21 (PMID: 32029743).
Over the last 7 years, a more detailed picture of how extra genetic material affects gene regulation and the impact on DS has emerged. For example:
- Gene expression patterns in fibroblasts and induced pluripotent stem cells (iPSCs) derived from identical (monozygotic) twins discordant for trisomy 21 (a very rare event) showed that precise domains of gene dysregulation were distributed across all chromosomes, not just chromosome 21, and that they correlated with other markers of chromatin accessibility (PMID: 24740065).
- Comparing DS-specific methylation patterns in cells from brains and lymphocytes of fetuses and adults with DS to cells from control samples identified differences in transcription factor binding sites, suggesting a mechanism for the altered epigenetic pattern of gene expression in DS (PMID: 26607552).
- Evaluating specific genes and segments within the so-called “critical region” on chromosome 21, which is postulated to play an important role in cognitive impairment in DS, revealed that the genetic interactions within it are more complex than initially presumed (PMID: 26374847).
- Small changes in the dosage of many genes on an entire chromosome had a cumulative effect on the features of DS in an individual (PMID: 28388408).
Research has also examined mechanisms that contribute to nondisjunction, or the lack of chromosome separation during meiosis, resulting in aneuploidy or an imbalance in the number of chromosomes in an individual, as occurs in trisomy 21.
- Comparing chromosome nondisjunction in egg and sperm cells showed that the relative inefficiency of cross-over events in female oocytes may contribute to the increased rate of trisomy that occurs in eggs relative to sperm (PMID: 28262352).
- Evaluating genetic markers in children with DS and their parents allowed identification of candidate genes associated with maternal nondisjunction of chromosome 21, contributing to DS (PMID: 31830031).
- A novel approach to potentially improve outcomes in DS attempted to “silence” or turn off the extra copy of chromosome 21 by recruiting XIST, a molecule involved in X-chromosome inactivation in females. XIST “coats” the extra copy of chromosome 21 so it cannot be expressed. Silencing the extra copy of chromosome 21 allowed neural stem cells derived from individuals with DS to develop properly into neurons in culture (PMID: 31978324).
A number of studies have used mouse models of DS to explore the pathogenesis of co-occurring conditions:
- Tests of the response of heart rate and blood pressure to exercise and stress in the most commonly used Ts65Dn model of DS found that these parameters are similar to the autonomic dysfunction in humans with DS (PMID: 31496136).
- Other evaluations of murine models of DS identified genes that may contribute to the congenital heart defects present in one-half of infants with DS (PMID: 27029737).
- Murine models helped researchers characterize the neuropathological findings and learning and memory deficits in mice across the lifespan, from prenatal into adulthood, including cognitive decline in aging mice. These studies provide a framework for preclinical evaluation of potential treatments for the cognitive features of the condition (PMID: 25975229; PMID: 26230397; PMID: 26854932).
- Maternal choline supplementation in a mouse model of DS showed improvements in attention and learning in their offspring from this in utero treatment (PMID: 27840230).
Cellular models utilizing primary cultures and iPSC lines derived from individuals with DS have helped explain aspects of neurodevelopmental impairment and neurodegeneration in DS:
- Overexpression of the OLIG2 gene in ventral forebrain neural progenitor cells from individuals with DS produced excessive numbers of inhibitory interneurons and impaired memory tasks in DS chimeric mice. This effect was rescued by knocking down the OLIG2 overexpression (PMID: 31130512).
- Mitochondrial turnover deficits in fibroblasts from individuals with DS suggested the involvement of the mTOR pathway, important in cell turnover, as a potential therapeutic target (PMID: 31332166).
- Although astrocytes typically support and protect neurons in the brain, in DS, they exhibited higher levels of reactive oxygen species and lower levels of factors that promote neuronal function and formation of synapses (PMID: 25034944).
- Human iPSCs can form three-dimensional structures known as cerebral organoids, which mimic the cortical organization of a primitive brain, and have been used to model features of Alzheimer’s disease (AD) in both familial and DS forms of dementia. These organoids demonstrated findings similar to amyloid plaques and neurofibrillary tangles that are classic for AD (PMID: 30171212).
- The case of an elderly man with DS and partial trisomy of chromosome 21 who only had 2 copies of the amyloid precursor protein (APP) gene and who showed no clinical, biochemical, or neuropathological findings of AD at death established that three copies of the APP gene on chromosome 21 are required in the pathogenesis of AD in DS (PMID: 27983553).
- In cultured neurons from rat and mouse brains, and cells from individuals with DS, excess APP impaired certain cellular functions vital to neuronal survival, thereby linking the pathogenesis of AD in DS to APP levels in sporadic cases (PMID: 31043483; PMID: 27064279; PMID: 28851452).
Epidemiological studies of DS in humans revealed factors that contribute to the risk of co-occurring conditions in DS and provided information about their outcomes. In some cases, these findings will allow physicians to tailor management strategies and optimize outcomes, thereby improving quality of life for these individuals. For example:
- Multiple researchers identified genes that increase the risk of congenital heart disease (CHD), including atrioventricular septal defects, in newborns with DS (PMID: 33093519; PMID: 26194203).
- For infants with DS, CHD, and only a single heart ventricle (rather than two), certain clinical features predicted better outcomes after surgery (PMID: 26867706).
- The incidence and severity of obstructive sleep apnea (OSA) in infants with DS was higher in those with gastrointestinal complications and heart defects (PMID: 25604659).
- Most infants with DS are screened for CHD in infancy, and those without it are assumed to have healthy hearts. However, researchers found that up to 6 percent of previously healthy, asymptomatic children and adolescents with DS between ages 10 years and 20 years had an unsuspected cardiac diagnosis, suggesting that periodic rescreening may be of value in this group (PMID: 31588666).
- Research identified genes that contribute to the increased risk of acute lymphoblastic leukemia (ALL) in children with DS (PMID: 24747640; PMID: 31350265). A separate effort showed that the best outcomes for ALL treatment resulted when the dose of chemotherapy was lowered to reduce the risk of infections and other complications (PMID: 24222333).
- Sex differences in the risk of developing AD in the general population did not exist in adults with DS, who demonstrated equal prevalence of AD in men and women with DS (PMID: 32995462).
DS-Related Conditions: Screening, Diagnosis, and Functional Measures
Nearly 200 papers published in the past 7 years have addressed screening, diagnosis, and functional measures of co-occurring conditions in individuals with DS. As uptake of prenatal diagnosis of DS has increased, researchers have refined existing technology and developed novel imaging approaches to enhance prenatal identification of co-occurring conditions in DS. For instance:
- Techniques that utilize cell-free fetal DNA from maternal blood samples, typically obtained at around 10 weeks gestation, have advanced non-invasive prenatal screening (NIPS) for DS (PMID: 23765643).
- Using single-nucleotide polymorphism-based NIPS assays improved technical sensitivity and specificity in identifying aneuploidy conditions such as DS (PMID: 25004354).
- In surveys, mothers of children with DS reported that they were likely to use NIPS in the future. They also felt that NIPS was likely to lead to more terminations of pregnancies affected with DS, and recommended that more balanced and objective information be provided about DS at the time of diagnosis (PMID: 24481673).
- Novel technology based on genomic profiling of fetal trophoblast cells from cervical samples obtained by Pap smear as early as 5 weeks of gestation showed promise in screening (PMID: 27807286).
- Additional prenatal studies of conditions associated with DS can help families and medical providers anticipate the care needs for these infants. For example, researchers:
- Evaluated brain growth in utero to characterize neurodevelopment in fetuses with DS (PMID: 31264685)
- Confirmed that the radiographic “double bubble” sign on ultrasound can predict duodenal atresia in newborns with DS (PMID: 31167209)
- Determined features of prenatal lung and vascular development in DS that may predispose newborns to pulmonary arterial hypertension (PAH) (PMID: 27487163)
For some co-occurring conditions in DS, diagnosis is most typically made in infancy. Research on these conditions has found the following:
- Certain factors influenced infant’s risk of developing PAH beyond the newborn period. Although it was often transient, and associated with CHD, PAH was more likely to occur in children with DS who also had OSA, hypoxia, and frequent pneumonia (PMID: 30025669).
- Swallowing and feeding problems are common in infants with DS, leading to potential complications, such as aspiration, pneumonia, and failure to thrive. One retrospective chart review project revealed that more than one-half of infants had some degree of oral and/or pharyngeal phase dysphagia during a videofluoroscopic swallow study, the test typically used to make a diagnosis, and nearly 40 percent required some feeding modifications to prevent aspiration (PMID: 30588741).
- Hypothyroidism occurred more frequently (32 percent) in infants with DS than suggested by previous estimates (15 percent) based on newborn screening results alone, reinforcing the value of retesting infants at 6 months of age (PMID: 24945161).
- A retrospective records review of more than 500 children with DS found that thyroid disease can persist into childhood, with approximately one-quarter of the children demonstrating hypothyroidism, mostly autoimmune (PMID: 28259872).
Heart defects, including CHD, are identified in about one-half of infants with DS. Overall, the following studies suggest that although infants with DS have worse outcomes for some less common types of CHD and may exhibit developmental delays in infancy, many of them recover with regard to cognitive abilities by school age.
- An evaluation of long-term outcomes after single-ventricle palliative procedures found that children with DS had lower 10-year survival (67 percent) than controls without DS (92 percent) for this particular lesion (PMID: 31332952).
- Among infants with DS and atrioventricular septal defects, a more common form of CHD, neurodevelopmental outcomes were impaired at 12 months to 14 months of age. Mothers of these infants reported increased levels of emotional stress (PMID: 25683160).
- Infants with DS and CHD who had surgery in the first year of life (PMID: 26914309) demonstrated poorer neurodevelopmental outcomes in receptive, expressive, and composite language than children with DS without CHD. However, by school age, there were no differences in IQ, language, or academic achievement scores between the two groups (with DS and with or without CHD).
Birth defects registries have pointed to the increased risk of specific types of cancer, specifically leukemias, in children with chromosomal disorders such as DS (PMID: 31219523), but the reasons for this increased susceptibility have not been clear. Studies published during the past 7 years have elucidated the following:
- Acquired mutations in the GATA1 gene in development of transient abnormal myelopoiesis (TAM) in DS as well as additional genetic changes predisposed those with DS to developing acute myeloid leukemia (AML) (PMID: 31303423; PMID: 25533034).
- Children’s Oncology Group-led studies identified the distinguishing diagnostic characteristics of TAM and AML in children with DS and the treatment strategies that improve outcomes while reducing toxicity for these children (PMID: 28389462; PMID: 31429606).
- Research reported outcomes of children with a particular form of ALL, more common in DS, as well as potential therapies that may improve their prognosis (PMID: 25049327).
Poor sleep can be a significant health issue for children with DS. The following studies show that sleep disturbance is common across the lifespan in DS, that it can impact cardiac outcomes, and that interventions for OSA may be beneficial.
- Two different studies used the Children’s Sleep Habit Questionnaire (CSHQ) to identify sleep problems in more than 60 percent of enrolled children with DS. The risk for sleep problems was amplified in those with asthma, autism, and enlarged tonsils and adenoids (PMID: 24733987; PMID: 26105013).
- In a cohort of infants and young children with DS, researchers used home actigraphy recordings to demonstrate that general sleep quality was poor in these children, but that circadian rhythm and phase were preserved (PMID: 28449894).
- Across the lifespan, sleep-disordered breathing and hypoventilation were very common in DS, and OSA increased significantly with age and Body Mass Index (BMI). Central apnea was more common in infants and toddlers (PMID: 28665356).
- Severe OSA was associated with cardiovascular dysfunction, but improved with the use of continuous positive airway pressure (CPAP) during sleep (PMID: 26847969).
In people without DS, obesity is often correlated with OSA and other significant risk factors for cardiometabolic disease, but the relationship between these factors in people with DS is less well understood. Several publications since the last DS research plan provide some emerging data about the complex relationships among BMI, OSA, and cardiovascular health in DS.
- Compared to controls matched by age, sex, race, ethnicity, and BMI, youth with DS were more likely to have altered lipid profiles and evidence of pre-diabetes in spite of having less visceral fat (PMID: 31315916).
- Although DS-specific growth charts, including BMI charts, exist and were informed by research, the DS-specific BMI charts are less sensitive than the BMI charts for the general population. As a result, adiposity in children with DS who are 10 years of age or older is undercounteded when using the DS-specific charts (PMID: 27630073).
- In adults with intellectual disabilities, the prevalence of obesity was higher than in the general population, and this risk was magnified in females and in those with DS (PMID: 24256455).
- Because obesity negatively impacts most domains of weight-related quality of life measures in youth with and without DS, many investigators recommended that healthcare providers address weight issues in youth with DS (PMID: 28751125). However, more recent studies of aortic stiffness and other measures of cardiovascular function in adolescents with DS showed that cardiac function did not correlate with actual risk of cardiac events, such as heart attacks, as compared to the general population (PMID: 31201031).
A number of published studies describe neurodevelopmental and cognitive impairments in DS as well as standardized approaches to measure them.
- Researchers validated the NIH Toolbox Cognitive Battery for use in children with intellectual disabilities and demonstrated specific cognitive profiles in children and adolescents with DS (PMID: 27602170).
- Using the Social Responsiveness Scale to measure the range of social communication impairments in adolescents with DS without a co-occurring diagnosis of autism found that many had elevated scores in some domains associated with autism, suggesting that DS-specific norms should be developed to improve the identification of those with true autism (PMID: 25657824).
- Infants with DS born at earlier gestational ages had higher rates of attention-deficit/hyperactivity disorder (ADHD), known to be common in people with DS (PMID: 33230240).
- Children with DS showed impairment in working memory, planning, and inhibitory control compared to matched children of comparable mental age who did not have DS (PMID: 25007296).
- Children with DS and infantile spasms had poor neurodevelopmental outcomes, with scores on cognitive, motor, and language all 20 points lower than infants with DS without spasms (PMID: 26523121).
- A comprehensive evaluation of the motor speech disorders, including ataxia and dysarthria, found in 98 percent of adolescents with DS (PMID: 31221009), showed that these disorders contributed to a lower speech intelligibility (percentage of intelligible words in conversation) (PMID: 31221010).
Vision can also be impacted in DS, and refractive errors requiring eyeglasses are common. Vision-related research findings include the following:
- Researchers evaluated the best method for measuring visual acuity in those with DS (PMID: 31157125).
- Keratoconus, a structural disorder of the cornea that can lead to loss of vision, is highly associated with DS (PMID: 26707415). Between 12 percent and 21 percent of study participants with DS exceeded the cutoff for detection of keratoconus, even though most had moderate rather than severe disease (PMID: 31479021).
- Using a comprehensive battery of visual function tests, researchers noted many similarities between the visual deficits seen in adults with DS and those with AD (PMID: 23784802).
Several published papers characterize the unique impact of trisomy 21 on the immune system.
- Transcriptome analysis in cell lines derived from individuals with DS revealed that trisomy 21 upregulates the interferon pathway, which can contribute to autoimmune problems and a reduced ability to combat certain infections (PMID: 27472900).
- Metabolome studies of blood plasma and cerebrospinal fluid from people with DS showed elevated levels of two metabolites produced with interferon stimulation, which may be damaging to neurons (PMID: 31628327).
- Multiple studies described the mechanisms that underlie the hyperactive immune system in DS. Findings suggest that drugs known as JAK inhibitors, which counteract increases in interferon, might be effective treatments.
Studies of aging individuals with DS showed the following:
- Studying plasma, neuroimaging, retinal amyloid imaging, and cognitive measures in adults with DS helped monitor the trajectories of AD biomarkers in this population (PMID: 26441570).
- A review of death records found that although heart disease, dementia/AD, and cancer were common causes of death, they were especially prominent at younger adult ages in those with DS; older adults with DS were more likely to die from influenza, pneumonia, respiratory failure, and choking (PMID: 32680774).
- Computer modeling showed that the benefits of screening mammography in women with DS were much less than in average-risk women, given the former’s overall lower breast cancer risks and shorter life expectancy (PMID: 31385214).
These discoveries demonstrate the evolution of the field of DS research to promote refinement of many of the approaches to screening, diagnosis, and measurement of co-occurring conditions across the lifespan, with the recognition that until a disorder can be accurately measured in a population, it cannot be treated. Furthermore, these studies show that there are differences in the identification and natural history of many of these conditions in DS, in comparison to the general population, that require a nuanced approach to their diagnosis and care.
Treatment and Management
Scientific efforts and advances that focus on medical management of DS continue to increase steadily. Since 2011, commercial laboratories have made NIPS-based methods for DS routinely available, evaluating cell-free fetal DNA markers from a maternal blood sample obtained in the first trimester. Researchers are further refining NIPS and its use.
- One study determined that, after receiving complete prenatal testing information via an interactive decision-support tool, pregnant women had improved knowledge regarding prenatal testing, age-adjusted DS risk, and risks of amniocentesis-related miscarriage (PMID: 25247517).
- A 2016 retrospective study showed that when the NIPS assay suggested a trisomy (such as DS), the results were sensitive for DS but diagnostic confirmation via additional testing was still recommended (PMID: 27371353).
- In 2020, the International Society for Prenatal Diagnosis published a position statement about first-trimester screening for DS in pregnancies with multiple fetuses (twins and triplets) using cell-free DNA; although this screening had not been previously recommended, the available evidence had sufficiently high-detection and low false-positive rates to support it (PMID: 33016373).
Earlier prenatal diagnosis of DS raises the possibility of in utero treatments that might improve cognition and other features of DS, although such studies would need to be pursued in a rigorous and ethically responsible manner (PMID: 28004394).
- Maternal choline supplementation improved cognitive function and protected forebrain neurons in affected offspring in a mouse model of DS (PMID: 26391046).
- Prenatal treatment with epigallocatechin-3-gallate (EGCG), a green tea extract that inhibits a gene on chromosome 21 known as Dyrk1a, reduced craniofacial development problems in a mouse model of DS (PMID: 28172997).
- A systematic evaluation of gene-expression data from human and mouse fetal DS samples identified drugs already approved by the U.S. Food and Drug Administration (FDA) that could rescue the abnormal transcript patterns (PMID: 27586445). The researchers identified an antioxidant, apigenin, that improved cognitive development, memory, and inflammation in a mouse model of DS when administered pre- and postnatally (PMID: 33098770).
- Researchers are exploring attitudes of parents of children with DS toward the hypothetical use of prenatal therapies to silence the extra chromosome 21 or medications to improve aspects of cognition (PMID: 31877259).
Studies also focus on management strategies and surgical interventions, when appropriate, for children with DS and CHD and OSA. Findings showed that surgical repair of heart defects in infants with DS had a significant impact on survival and positive outcomes; in contrast, medical and surgical management of OSA was more variable with regard to outcomes and evaluation.
- A landmark review, published in 2014, found that of 2,399 infants born with complete atrioventricular septal defect, 78 percent of whom had DS, who had surgery early in their first year of life, had generally good outcomes. Infants with DS had lower rates of death and major complications in the study than infants without DS (PMID: 25125206).
- A retrospective chart review identified children with OSA and/or behavioral sleep disturbances. Despite high rates of reported sleep problems, less than one-half underwent formal sleep study, called polysomnogram (PSG), but about 80 percent of those with sleep problems received sleep intervention (PMID: 27541580).
- Adherence to the nighttime CPAP appliance among children with OSA was only approximately 50 percent, but compliance was higher in those with developmental delay, and in females with DS (PMID: 27092702).
- Management approaches to OSA in children without enlarged tonsils required more evidence to refine the use of oral appliances and CPAP in children with DS (PMID: 26598935).
- A study on the impact of 2011 guidelines, which recommended a pre-surgical PSG before adenotonsillectomy (removal of adenoids and tonsils), found that high-risk populations, including those with DS, were more likely to have a pre-surgical sleep study after the guidelines were published (PMID: 32427548).
Advances in treatments for children with DS and leukemia have led to refined chemotherapy approaches that optimize survival and minimize relapse.
- Survival rates for children with DS and AML were high, but these children were more likely to have chronic health conditions that impacted quality of life than children without DS who had survived AML (PMID: 27906794).
- In children with standard-risk ALL, the total tolerated dose of methotrexate was lower in those with DS because of an increase in side effects, such as mouth sores. Otherwise, children with DS and standard-risk ALL had excellent survival rates (PMID: 31160295).
- Children and adolescents with DS and ALL had similar rates of remission and relapse to those without DS, but higher rates of toxicity, such as infections (PMID: 29878490).
- Among survivors of both types of childhood leukemia, those with DS were more likely to have serious chronic health conditions than those without DS, but the DS group also had a decreased risk of secondary cancers (PMID: 29105081).
- An experimental method of chromosome silencing in human fetal blood cells restored normal blood cell development (PMID: 30518921); although the approach is not feasible for treating DS-related leukemias, it remains a tantalizing area of research.
Several studies have evaluated strategies to improve speech development and communication in children with DS.
- Language development was enhanced when children with intellectual disabilities, such as DS, gestured at objects before they were able to label them, and when parents then translated these gestures into words (PMID: 26362150).
- Providing families with feedback on child progress across early skills, such as vocalizations between young children with DS and their parents, increased child vocalizations and conversational exchanges for those with DS compared to typically developing peers (PMID: 24686777).
- A study on the elements of speech intelligibility in children and adults with DS showed that the ability to be understood increased with age for children with DS, especially between the ages of 4 and 16 years. These findings have implications for future assessment and intervention strategies (PMID: 29214307).
- In the context of expressive language skills among adolescent males with DS, family-related factors, such as closeness of the mother-child relationship, over time provided some protection from reduction in the quality of language exchanges (PMID: 32593286).
- Multiple strategies helped children with DS access and efficiently use Augmentative and Alternative Communication to further improve their communication skills (PMID: 31398294; PMID: 31697898).
In the context of efforts focused on motor skills, researchers made the following discoveries:
- The use of a modified, electric-powered ride-on car encouraged mobility and socialization for children with developmental delays, including DS. The research team tested whether infants with DS could use the car to develop independent mobility during regular at-home driving sessions, and found that most of the tested infants enjoyed the experience and had improved social and motor skills (PMID: 30557294).
- After adults with DS completed a 12-week exercise intervention, participants had improved performance on two measures of memory, suggesting that physical exercise may help maintain aspects of cognition and memory in individuals with DS as they age (PMID: 29501470).
Taken together, these studies and reports provide evidence of advances that can improve quality of life across the age spectrum for individuals with DS.
DS and Aging
Since the last NIH DS research plan was published, researchers have made a great deal of progress in understanding the aging progress in DS, and studying the progression of symptoms from Mild Cognitive Impairment (MCI) to AD dementia has been an area of focused study in this high-risk population. In 2015, investigators, advocacy and research organizations, and NIH institutes and centers came together to set a roadmap for studies of AD in DS (DS-AD) (PMID: 25510383; PMID: 32544310). Emerging evidence also suggests many similarities in the development of MCI and AD between the high-risk aging DS population and the general population. Additional progress includes the following:
- Based on California Medicare claims data to characterize the frequency of AD in the aging adult population (older than 45 years of age) with DS, nearly 50 percent those 65 or older had a dementia diagnosis. Many adults with DS also had several co-occurring, but treatable conditions (PMID: 30032260).
- Researchers used Medicaid claims data from the state of Wisconsin (PMID: 31657825) to further describe the epidemiology of DS-AD. The study found that the prevalence of dementia claims rose from 19 percent in the 40- to 54-year-old cohort to 52 percent in those age 55 years or older, similar to rates of dementia observed in the clinical setting.
- A molecular “signature” study of aging showed that blood and brain tissue from adults with DS were an average of 6.6 years older than cells from adults without DS of the same age (PMID: 25678027).
- Scientific work using animal models, such as the Ts65Dn mouse, also revealed new information about disease progression. This mouse model exhibits age-related memory loss coupled with neuronal degeneration, in part related to triplication of APP, and increased deposits of amyloid in the brain, a hallmark of AD (PMID: 27538963).
- Disruption of signaling in neurons in the locus coeruleus, a specific portion of the brain associated with working memory, learning, and attention, caused inflammation and memory loss in this mouse model (PMID: 31678403).
- Chronic administration of an agent that treats neural inflammation in middle-aged Ts65Dn mice reduced typical memory loss, inflammatory cytokines, and microglial activation (PMID: 31944407).
- Inhibition of an enzyme known as BACE1, which cleaves APP, reduced the deposition of amyloid in the brains of a different mouse model of DS, indicating the potential value of BACE1 modulation as a therapeutic target to prevent neurodegeneration in DS-AD (PMID: 26923405).
- Injecting extracts of the tau protein, part of the neurofibrillary “tangles” observed in AD brains, from the brains of adults with DS-AD into the brains of transgenic mice that overexpress tau resulted in spread of neurofibrillary tangles and eventual loss of neurons (PMID: 25534024).
- Brains from individuals with DS-AD demonstrated tau phosphorylation and abnormal processing before the development of neurofibrillary tangles. The finding confirmed the association with AD in those with DS (PMID: 24033439), similar to the disease course in those without DS.
One of the challenges in studying DS-AD is accurate assessment of progressive dementia within a population that already has a broad range of baseline intellectual disability. Creating measures to document the transition from MCI to AD is critical to understanding the evolution of DS-AD, and for the development of therapies.
- Researchers successfully adapted an instrument that is currently used in the general population, by all federally funded Alzheimer Disease Research Centers (ADRCs), for use in adults with DS. The instrument captures a range of cognitive impairment in adults with DS that can then be used to track progression of AD in this population (PMID: 31842726).
- The National Task Group-Early Detection Screen for Dementia, a measure developed to assess MCI and dementia in those with intellectual disability, proved to be a useful tool for evaluating dementia status in a sample of 185 adults with DS (PMID: 33314467).
- The role of APP, tau, and neuroinflammation in AD progression among adults with DS seemed to be similar to that in familial and sporadic AD in those without DS, a finding that may facilitate development of treatments in both populations (PMID: 30733618).
The Alzheimer’s Biomarker Consortium-Down Syndrome (ABC-DS) project (see Program Portrait 4) has yielded many important insights into the role of aging in DS. Funded since 2015 by NIH, two groups of investigators have recruited nearly 500 participants with DS, older than 25 years of age, to study cognitive measures, neuroimaging findings, genetic markers in biological specimens, lifestyle, and environmental factors that predict risk and resilience for development of AD (PMID: 32058812).
- Neuroimaging findings measuring positron emission tomography tracer PiB showed that β-amyloid accumulation is associated with declining cognitive functioning in adults with DS who have preclinical AD (PMID: 28715661).
- Adults with DS also had a loss of gray matter volume and reduced brain glucose utilization with development of AD (PMID: 29254096).
- Cerebrovascular disease, characterized by cerebral amyloid angiopathy and microbleeds seen on brain pathology, was more common in adults with DS who had symptoms of AD (PMID: 29195510; PMID: 30452414).
- Disrupted sleep was associated with amyloid accumulation and cognitive features of preclinical AD, suggesting that aspects of lifestyle may be modifiable risk factors for dementia in adults with DS (PMID: 32447011).
Exploration of AD biomarkers in blood plasma and cerebrospinal fluid (CSF) from adults with DS revealed some of the most significant findings:
- Plasma and CSF biomarkers of amyloid, tau, and neurofilament light protein had good diagnostic performance for detecting AD in adults with DS, and may have utility for the early detection of AD in these individuals (PMID: 30172624).
- Plasma proteomic (PMID: 32435687; PMID: 32626817) and metabolomic (PMID: 32258359) signatures helped predict MCI and later AD development in those with DS as they age, and similar biomarker profiles in CSF provided additional insights (PMID: 32671183). These studies and many others point to the potential to use such biomarkers in clinical trials to prevent and/or treat AD in DS (PMID: 34942129).
Research Infrastructure
In the domain of research infrastructure, a number of resources have been created to support scientific inquiry. New animal and cellular models of DS have helped to understand the basic biology that underlies the condition. By collecting information about individuals with DS, tools such as registries and outcome measures can elucidate the prevalence of co-occurring conditions in DS and support development of treatments and interventions for these co-occurring conditions (see Program Portrait 2).
- Although brain development, gene expression, and behavioral phenotypes have been characterized prenatally and postnatally in several well-known mouse models (PMID: 29716957), researchers created and characterized an entirely new mouse strain, the TcMAC21 mouse (PMID: 32597754), that may serve as the most complete genetic mouse model of DS to date. This strain contains an extra copy of human chromosome 21 with a mouse centromere, to maintain fidelity of segregation in daughter cells, and it replicates many phenotypes found in the human condition.
- Additional exploration of chromosome 21 genes in zebrafish (PMID: 29760202) and worms (PMID: 29367452) may allow improved understanding of the functional impacts of trisomy on critical genes conserved across many species and provide insights into understanding development of DS in humans.
- Researchers using human stem cells have capitalized on the value of re-differentiating iPSCs into neural and glial derivatives to understand neurodevelopment (PMID: 32058817); in addition, methods to create 3-D spheroids can be used to model more advanced brain development in DS.
- A brain transcriptome developmental atlas demonstrated that many genes associated with oligodendrocyte differentiation, which is critical for myelination and white matter development, were dysregulated in DS (PMID: 26924435).
- Methylation pattern comparisons of brain and other tissue samples from individuals with DS and controls shed light on differentially methylated regions of the genome and provided a resource to understand epigenomic gene regulation in a tissue-specific manner (PMID: 31010359).
- Publication of revised U.S. growth charts specifically for children with DS enhanced understanding of height, weight, and BMI. These charts will allow better longitudinal tracking of children up to 20 years of age with regard to health and nutritional status.
- An NIH-sponsored workshop held in 2015 described standardized outcome measures, particularly in the domains of cognition and behavior, for use across future clinical trials (PMID: 28452584). Likewise, robust biomarkers to track disease progression are viewed as essential for designing and developing treatment trials to potentially prevent DS-AD (PMID: 32506291).
- A neurodevelopmental assessment tool, the Arizona Cognitive Test Battery, developed specifically for DS, demonstrated adequate levels of reliability to monitor cognitive changes over time for young participants in clinical trials (PMID: 28452581).
- Feasibility, reliability, and validation of cognitive measures within the NIH Toolbox were assessed for children and young adults with intellectual disability, including DS, leading to refined measures for this population (PMID: 32094241).
- DS-Connect®: The Down Syndrome Registry, launched in 2013 by the Eunice Kennedy Shriver National Institute of Child Health and Human Development (NICHD) to enhance recruitment of individuals with DS and their family members for DS research projects, passed the 5,000 participants mark; some of these participants reside outside the United States (PMID: 26271554).
Goals and Objectives: NIH INCLUDE/DS Research Plan
A. Basic Research
Our understanding of DS has significantly expanded since 2000, when investigators published the full DNA sequence of chromosome 21. It is now possible to identify all of the genes present in triplicate in those with DS and, ultimately, to understand the effects of having an extra copy of individual genes or clusters of genes. Today, researchers use model systems, tissues, and new technologies to study these effects.
Expand Basic Research Approaches
- Conduct mechanistic studies on the links between chromosome 21 and cognition, including identifying the genes involved in neurodevelopment, developmental signaling pathways, and multiple mechanisms of stress. Sequence the events that lead to abnormal dendritic (neuronal) spine development, including genetic and cellular aspects.
- Use available and new technologies, including neuroimaging, electrophysiology, histopathology, metabolomics, iPSCs, and studies of the microbiome, to define nervous system development and function in DS.
- Define the impact of sex on dysregulation of genetic and cellular mechanisms.
- Expand genetic and epigenetic profiling beyond chromosome 21 to elucidate complex gene-network effects.
- Study pathways that affect mitochondrial function and use genomics, such as interrogating mitochondrial genes and their possible interactions with genes on chromosome 21, to identify dysregulated pathways, including those related to oxidative stress, that may lead to abnormal organ structures.
- Examine the function, development, and differentiation of both B cells and T cells in individuals with DS.
- Explore the role of interferons and how they drive innate and adaptive immune function and dysfunction. This work may include:
- Research that could lead to standardized phenotyping of the immune system in individuals with DS, including cell functional assessment, the genetics of immune disorders, and the trajectory of dysregulation and disease, such as what trisomy 21 mechanisms may increase the risk and/or severity of autoimmune conditions in people with DS
- Genome-Wide Association Studies (GWAS) to determine whether gene variants predispose people with DS to autoimmune conditions, such as thyroid disease
- Study the cellular mechanisms for and role of inflammation in people with DS, including inflammation present in tissues and organs.
- Study the impact of trisomy 21 on diverse human tissues, using iPSCs, differentiated cells and organoids derived from iPSCs, morphogens, and monolayer cultures.
- Use brain tissue samples to help define the genome, epigenome, metabolome, transcriptome, and proteome in DS.
- Obtain microbiome (gut, oral) data from people with DS to help understand the potential associations of the microbiome to commonly co-occurring conditions in DS.
- Explore the role of inherited genomic variation in DS across different age groups to improve cancer screening, diagnosis, and stratification for treatment, particularly for children.
- Determine whether there are genetic variants that modulate the impact of leukemogenic genes on chromosome 21 to help define the risk of developing hematological disorders, such as leukemia.
- Study the genetic and non-genetic risk factors for health conditions related to vision in people with DS, and whether there are predisposing risk factors for these conditions that can be identified during pregnancy.
- Study the mechanisms by which trisomy 21 increases susceptibility to and/or severity of infectious diseases in people with DS, such as whether any specific genes or signaling pathways may be implicated.
- Study the mechanisms by which trisomy 21 increases the risk for different types of diabetes, such as whether any specific genes or signaling pathways may be implicated; obtain lipidomic and other ‘omics data to understand risk of diabetes and obesity in people with DS.
- Study the impact of dysregulation of pathways/hormonal circuits that regulate weight, energy metabolism, and appetite control.
- Obtain metabolomics data, both general and tissue-specific, to establish metabolic phenotypes and discover new biomarkers of metabolic disease.
- Define the role of trisomy 21 on metabolic pathways that may modulate the onset and severity of musculoskeletal conditions, such as arthritis.
- Explore molecular and cellular bases for resilience versus the susceptibility of premature aging in DS.
- Create an integrated dataset by combining genomics, proteomics, and metabolomics data to advance understanding of the fundamental biology of DS.
Expand Basic Research on Alzheimer’s Disease in Down Syndrome (DS-AD)
- Study molecular and cellular mechanisms of AD to identify biomarkers for this condition. This activity may include efforts to:
- Define epigenetic changes and hormonal changes across the lifespan in models of DS-AD to help standardize clinical and genetic phenotyping.
- Define DS-AD risk alleles and compare them to those for sporadic AD.
- Develop models of the genetic basis, mechanisms, and significance of dysregulated endosomes, exosomes, autophagosomes, and proteostasis in aging and DS-AD.
- Elucidate conformation and toxic mechanisms of aggregating proteins, such as beta-amyloid and tau, from human tissue in DS-AD.
- Create and compare models to assess the impact of other human chromosome 21 genes on aging and DS-AD.
- Define differences and similarities between models of DS-AD versus late-onset AD and early onset, familial AD.
- Explore the effects and mechanisms of amyloid angiopathy and breach of the blood-brain barrier in DS-AD.
- Explore the role of the microbiome on AD pathology in DS.
Develop Model Systems for DS-AD Research
- Conduct comprehensive ’omics studies of aging and AD in a wide range of models, including yeast, worm, fly, zebrafish, mouse, rat, non-human primate (NHP), and human cell models.
- Examine telomeric length and regulation in mouse models versus human cell lines.
- Define age-related changes in neurons, glial, and endothelial cells in mouse and human models.
- Define the role of age-related hormonal changes on DS-AD endotypes and phenotypes in mouse models.
- Study the origins and consequences of autoimmune conditions in a mouse model of DS.
- Define in vivo mechanisms in model systems that reflect clinical phenotypes in DS, particularly prenatal developmental studies that cannot be conducted in humans.
- Define and compare genetics, mechanisms, and significance of dysregulated endosomes, exosomes, autophagosomes, and proteostasis in DS animal models.
- Conduct research in a model of inducible silencing of the entire chromosome 21, or of specific genes on chromosome 21.
- Continue to analyze synaptic function in a DS mouse model, focusing specifically on relevant genes also located on human chromosome 21.
- Complete comparative phenotyping, including aging and lifespan of all DS mouse models, to inform the development of phenotypes in people with DS.
Program Portrait 1: Basic Research
Brain Development in DS
Basic biomedical research aims to uncover and understand mechanisms involved in typical development and function and in diseases and conditions such as DS. By examining developmental and other changes associated with DS, researchers hope to identify new ways to improve health and quality of life for people with this condition. Multiple NIH ICOs support basic research on DS, reflecting its effects on multiple organ systems across the lifespan.
For example, the National Institute of Neurological Disorders and Stroke (NINDS) supports research to understand mechanisms of brain development in DS that lead to intellectual disability, as well as the longer term effects on cognition. In one recent study, researchers used a multidisciplinary approach to show that a defect in the integrated stress response (ISR), a signaling pathway that controls the balance of protein production and destruction inside cells, contributes to cognitive impairment and altered neuronal function in a mouse model of DS. Experimentally suppressing the ISR improved measures of long-term memory in the mice, suggesting that this signaling pathway may be a promising therapeutic target (PMID: 31727829; funded by NINDS, the National Human Genome Research Institute, and the National Cancer Institute).
In another study, researchers sought to understand the mechanisms behind the imbalance of inhibitory and excitatory brain activity observed in people with DS, and if and how this imbalance may contribute to intellectual disability. By studying iPSCs from people with DS, they found that increased expression of the OLIG2 gene leads to excess production of specific types of inhibitory neurons during early brain development. Decreasing the expression of Olig2 reduced this overproduction and improved behavioral deficits in mice, pointing to another possible strategy for future therapies (PMID: 31130512; funded by NINDS, NICHD, the National Institute of General Medical Sciences, the National Institute on Alcohol Abuse and Alcoholism, the National Institute of Environmental Health Sciences, the National Center for Advancing Translational Science, and the National Institute on Drug Abuse).
B. Cohort Development/Epidemiology
To perform studies in people with DS, researchers need groups—called cohorts—with enough people and information to appropriately inform the research. Developing these cohorts of people with DS is essential to following individuals’ development over time and performing deep phenotyping and natural history studies. For example, a map that includes comprehensive genomic, epigenomic, transcriptomic, and proteomic information will help scientists understand the predisposing risk and protective factors that underlie the highly penetrant features, those that are very common, in DS. Enrolling a cross-sectional cohort of individuals with DS—people of different ages, sexes, races, and ethnicities across the lifespan—will capture the broadest array of phenotypes and ages of onset for the co-occurring conditions, and will identify the critical windows for interventions. Longitudinal demographic and epidemiological studies will improve understanding of these co-occurring conditions in individuals over time and provide the basis for developing long-term social and health care policies for these individuals. Moreover, many of these co-occurring conditions also are common in people who do not have DS; therefore, findings from DS research will have implications for the health of the overall population.
Develop a Cohort(s) for DS Research
- Develop a cohort of individuals with DS across the lifespan, including older individuals (such as those born 1970 to 1990), and those from diverse socioeconomic backgrounds, cultures, and geographic areas, ensuring representation across all age, sex, and racial/ethnic population groups.
- Define the impact of race and ethnicity on trisomy 21, specifically addressing whether DS has a disparate impact on particular racial or ethnic populations. Include partial trisomy and mosaic DS cohorts in these studies, and acknowledge the wide variability in phenotypes among individuals with DS.
- Collect GWAS data on a subgroup—one large enough to provide statistical adequate power—of participants with DS from larger efforts, such as DS-Connect®: The DS Registry (see Program Portrait 2) or NIH’s All of Us research program, to develop valid genotypes and phenotypes.
- Conduct research on the health impact of low socioeconomic status and other social determinants of health in DS.
- Link cohorts to a sufficiently large number of biological samples (e.g., blood, hair, saliva) from people with DS through a federation of coordinated biobanks to allow detailed, longitudinal characterization (phenotyping) of individuals with DS. To achieve this goal, consider linking to existing cohorts, including those maintained internationally.
Conduct Longitudinal/Prevalence Studies of Co-Occurring Conditions in DS
- Expand longitudinal studies of the natural history of aging and DS-AD, beginning early in life. Conduct epidemiological studies of adults with DS to identify the onset and trajectories of co-occurring conditions and mortality related to AD, and ascertain the distribution, demographics, and survival rates of DS-AD, including complications of AD that may contribute to mortality (such as pneumonia). Examine the gender, race, and ethnic differences in DS-AD onset and progression.
- Examine environmental and behavioral factors (e.g., education, work, home settings) and risk factors (e.g., lifestyle, diet, exercise, sleep, substance use) to better understand the impact on cognition and body system function, including cardiovascular health.
- Chart the trajectory of sex differences and co-occurring conditions on the health of people with DS over time.
- Develop diverse cohorts for identifying and validating plasma biomarkers.
- Include assessments of cognitive, functional and motor skills (including executive function), speech/language and hearing, and behaviors (including validated methods to measure adaptive behaviors and successful independence) in conjunction with imaging and genetic biomarkers in longitudinal natural history studies.
- Examine the prevalence of neurological and psychological conditions in people with DS across the lifespan[1], including identification of variations by race/ethnicity, sex, and/or geography. Collect data on ADHD and Autism Spectrum Disorder (ASD); mental health disorders, such as depression, anxiety, and regression; and sleep/circadian rhythm patterns, including the impact of sleep disturbances on learning and cognition, in longitudinal studies of children with DS.
- Obtain data on the neurodevelopmental trajectories of individuals with DS.
- Conduct longitudinal studies to ascertain the prevalence of cardiovascular conditions in people with DS across the lifespan[2], and to understand the effects of aging and co-occurring conditions on the cardiovascular system, including evaluation of sex, race, and ethnic differences. Collect epidemiological data to identify potential protective and risk factors for heart disease (such as physical activity) throughout the lifespan, with the goal of informing best practices for treatment.
- Conduct studies to ascertain the prevalence of thyroid disorders in people with DS across the lifespan[3] and whether there are variations by age, race, ethnicity, sex, or geography.
- Study the prevalence of pulmonary conditions in people with DS across the lifespan[4], including differences by race/ethnicity, sex, and geography; risk and protective factors; and long-term impact on health and well-being.
- Establish the prevalence of and risk factors for thromboembolic and hemorrhagic stroke in people with DS across the lifespan.
- Determine the prevalence of conditions affecting the eyes and/or vision in people with DS across the lifespan.[5]
- Conduct studies to ascertain the prevalence of ear, nose, and throat conditions in people with DS across the lifespan.[6]
- Study oral and dental development, such as the eruption sequence of teeth, speech, language, and auditory development, and risk factors for dental caries and oral inflammation in people with DS.
- Conduct epidemiological research on the prevalence of cancers, including leukemias, in people with DS across the lifespan and particularly in childhood[7], and the survivability of these cancers as compared to the general population. Characterize neurocognitive, behavioral, and quality-of-life outcomes related to cancer therapy in people with DS, continuing through survivorship, to identify risk factors for poorer outcomes and targets for interventions.
- Conduct research to establish the prevalence of gut/gastrointestinal as well as liver/kidney/bladder conditions in people with DS across the lifespan[8], including identification of variations by age, race/ethnicity, sex, or geography. Conduct a longitudinal cohort study of dysphagia in children with DS.
- Conduct epidemiological research to establish the prevalence of skin conditions in people with DS across the lifespan.[9]
- Conduct natural history studies of musculoskeletal conditions in people with DS across the lifespan.[10]
- Conduct definitive epidemiological studies to establish the prevalence of diabetes in people with DS across the lifespan[11], including identification of protective and risk factors for these conditions.
- Compile data on the etiology and timing of metabolic/weight status changes in people with DS across the lifespan and the prevalence of secondary conditions associated with obesity.
- Study how the immune system matures in individuals with DS from infancy through adulthood, and how the process might differ from the same maturation process in those without DS. Conduct longitudinal studies to map the immune system, incorporating inflammatory markers, susceptibility to infections, and responses to vaccines.
- Study COVID-19 risk and mitigation strategies for people with DS, including differential effects of SARS-CoV-2 infection on people with DS across the lifespan, in various living settings. Conduct tailored studies of effective dosing and immune response to vaccines to prevent COVID-19 in people with DS.
Program Portrait 2: Cohort Development
DS-Connect®: The DS Registry
To augment research on DS, NICHD launched DS-Connect®: The DS Registry in 2013. This research registry, a collaboration among self-advocates, families, DS organizations and foundations, and NIH ICOs within the DS Consortium (see Appendix A: NIH-Led DS Groups), aims to facilitate information sharing among persons with DS, families, healthcare and service providers, and researchers by collecting demographic and health information about people with DS through a series of online surveys. This confidential, secure, and responsive website was translated into Spanish in 2019. As of 2021, nearly 5,100 individuals with DS were registered.
The DS-Connect® professional portal launched in 2014 to allow approved investigators, clinicians, and other qualified professionals to access the de-identified data collected through the registry. The professional portal offers three levels of access: 1) viewing aggregate, de-identified data or survey content only; 2) performing customized searches or statistical evaluation for analysis, publication, or presentation; and 3) working through the registry coordinator to recruit participants for research or clinical studies. As of 2021, more than 532 researchers had professional accounts.
Researchers have used registry data to develop studies on the etiology, natural history, and treatments for DS and associated conditions; recognize trends in health characteristics and identify medical needs of those living with DS; and determine feasibility and other features of research studies involving those with DS. The DS-Connect® Research Review Committee approves access and use of the registry data by investigators to recruit for studies and surveys. As of 2021, researchers successfully used the registry to recruit participants for over 60 clinical trials and research studies, including 9 funded under the INCLUDE Project.
The registry is also facilitating linkages with other research studies, using special codes and identifiers, to allow the INCLUDE Project to build a large, virtual DS cohort, which helps to achieve the goal of assembling a large study population of individuals with DS. This resource, called the INCLUDE Data Coordinating Center Data Hub, will also help researchers understand factors that may contribute to differential survival and co-occurring condition rates among different groups.
C. Clinical Research/Co-Occurring Conditions
At least one-half of all children with DS also have a co-occurring health condition that can contribute to intellectual, developmental, and physical problems. For example, leukemia and CHD during early childhood have the potential to significantly affect cognitive function and overall health status later in life, and both necessitate extensive medical intervention. Within the context of DS, determining the optimal windows for early therapeutics for individuals with DS presents an ongoing challenge for researchers, as does establishing the optimal doses of off-label and new therapeutic agents for this population. Studies of daily environments, such as those structured to facilitate specific language interventions for children with DS, may also provide information that helps researchers design biobehavioral interventions for improving cognition and daily-life functioning. Ultimately, this research will provide the evidence base for informing and expanding current clinical care guidelines established by the professional medical and behavioral societies for all age groups of people with DS.
Define DS Phenotypes
- Convene a panel of experts (including both clinicians and researchers) on DS to define DS phenotypes across the lifespan using available clinical and genetic data. Inform the development of updated clinical guidelines to improve care for people with DS by incorporating data on changes related to stages of life (e.g., inflammation and metabolism), and on age ranges when interventions for co-occurring conditions might be most effective.
- Identify DS phenotypes and genotype-phenotype associations, including behavioral and developmental milestones, to inform understanding of: the natural history of DS, beginning prenatally and including puberty and adulthood; the timing of and targets for interventions to improve cognition or intervene in regression; the evolution of communication skills; and pathologies that affect hearing, balance, and vision.
- Explore differences in utero to ascertain why spontaneous fetal loss occurs only in some cases of trisomy 21, whether the placenta can provide insights on these pregnancy losses, and when the aging process begins.
Improve Clinical Research and Therapeutics for Co-Occurring Conditions
- Leverage the unique opportunities that come from prenatal screening for DS as part of routine prenatal care, and understand the role of the placenta in the developing fetus. For example, identifying fetuses with DS in continuing pregnancies creates the possibility of offering prenatal treatment(s) to the pregnant woman to minimize certain aspects of the syndrome, such as CHD. Following these pregnancies could also provide new ways to study antenatal influences, including placental function, on fetal development.
- Conduct brain-related research to determine the anatomical and morphological impacts of trisomy 21, such as relative size of different brain regions, plasticity, synaptic pruning, myelination, and glial and neuronal function.
- Apply findings about early infant/childhood development to fetuses, infants, and children with DS. Tailor newly developed behavioral interventions for typically developing infants for infants with DS to take advantage of brain plasticity during early development.
- Increase the number of individuals with DS in controlled clinical trials of experimental therapeutics and medical devices meant for the general population, taking into account differences in drug metabolism (pharmacokinetics [PK] and pharmacodynamics [PD]) to establish drug safety, efficacy, and dosing in people with DS, and evaluate differential side effects (such as changes in toxicity). Support additional clinical research in people with DS to tailor dosing and fit of therapeutics and medical devices that are already available to the public. Collect data on the relative efficacy, side effects, and interactions of therapeutics in those with DS when multiple co-occurring conditions are being treated simultaneously.
- Conduct clinical research to assess the efficacy of interventions for improved cognition, communication, hearing and balance, and vision.
- Include people with DS in clinical trials of vaccines and treatments, including COVID-19 vaccines, as they become available.
- Include people with DS and their caregivers/supporters throughout the clinical research process, beginning with study design, and develop strategies to increase the participation of people with DS of different age, sex, race/ethnicity, and socioeconomic status in research.
- Consider developing public-private partnerships with biotechnology companies/pharmaceutical industry to test specific therapeutics for certain aspects of DS in people with DS.
- Harmonize clinical trial protocols, when possible, with international efforts to enable meaningful data sharing. Develop sustainable diagnostic protocols and early intervention procedures that could be used in low- and middle-income countries.
Expand Research To Understand the Impact of Common Co-Occurring Medical Conditions in DS on Cognition and Overall Health Outcomes
Note: Co-occurring conditions appear in italics in the following list.
- Examine co-occurring neuropsychiatric conditions, such as ADHD, ASD, depression, and developmental regression, by studying gene-brain-behavior connections, the effects of early interventions, and their long-term health effects. Study the psychological effects of untreated co-occurring conditions (such as skin problems) in people with DS.
- Study how a traumatic life change, change in health status, or event perceived as traumatic by a person with DS may affect mental health in people with DS. Conduct research on the effects of disaster/trauma (such as the COVID-19 pandemic) on people with DS, including loss of educational interventions, reduction in physical activity, and limits on social interactions, independence, and routine. Tailor existing therapeutic treatments for traumatic stress to the specific needs of people with DS.
- Define how early medical or behavioral interventions for leukemias alter the developmental trajectory in children with DS. Improve assessment and management of side effects experienced by people with DS during treatment (such as pain/nausea). Continue to refine treatments for leukemias in children with DS, including both chemotherapeutic agents and non-chemotherapy approaches.
- Compare markers in biological samples from individuals with cancer, both with and without DS, to look at tumor specificity and biological signatures in cancers. Study cancer subtypes in people with DS and in people who do not have DS.
- Characterize congenital heart conditions and cardiac function in individuals with DS, as well as the effects of various medical management approaches (including the risk of anesthesia for surgery), and examine the impact of differences in cardiovascular function, immune response, and hypertension across the lifespan, including factors that may protect from atherosclerotic disease. Study neurodevelopmental outcomes among the large proportion of children with DS born with congenital heart conditions; these outcomes may vary even among children with DS who have the same heart defects and receive the same treatments as typically developing children.
- Study immune system differences in, and risk factors and potential treatments for, co-occurring autoimmune conditions most common in people with DS[12], and define the full impact of autoimmunity on the health of people with DS, including possible autoimmune-related etiologies for other co-occurring conditions. Study whether treatment of autoimmune skin conditions may address other co-occurring autoimmune conditions. Conduct research to determine whether, in people with DS, having one autoimmune disorder predisposes them to other autoimmune conditions, and how this susceptibility may differ from that of individuals without DS who have autoimmunity.
- Describe more fully mitochondrial dysfunction in DS, and develop targeted therapies to address it. Study how failed mitochondrial function and related oxidative stress impact muscle physiology and the relationship between neurologic function, cognitive deficits, and AD.
- Conduct research on the long-term health impact of various types of diabetes, including whether having type 1 diabetes increases the chance of developing other autoimmune conditions, and whether early treatment of type 2 diabetes can reduce longer-term health issues, such as heart disease, stroke, vision problems, neuropathy, and kidney disease.
- Study the long-term health effects of obesity in people with DS, including: consideration of sex, race, ethnicity, and socioeconomic status; what interventions (such as diet and exercise) might assist in management; and why lipid levels in people with DS with obesity are often within a normal range.
- Study nonalcoholic fatty liver disease in people with DS to understand how liver dysfunction may contribute to other co-occurring conditions.
- Conduct research on nutrient absorption and metabolism in people with DS (sometimes called the gut-brain axis) to understand preventive and risk factors for celiac disease and related disorders.
- Conduct studies to determine more precisely the thyroid-stimulating hormone level at which hypothyroidism manifests; develop treatments for thyroid disorders in addition to standard thyroid hormone management.
- Study differential response to types of infections[13], as well as risk factors and potential treatments, for individuals with DS, including antibiotics, antiviral medications, preventatives (such as palivizumab for Respiratory Syncytial Virus [RSV] pneumonia), and vaccines. Study how infectious diseases may influence overall health, longevity, and quality of life of people with DS.
- Study the long-term impact of hematological disorders and their treatments on the health and development of people with DS.
- Study the long-term health impact of epilepsy and seizure disorders and their treatments for people with DS, including their role in AD progression.
- Study moyamoya disease to improve early detection, develop biomarkers for the condition, and determine risk of stroke associated with the disease.
- Study hypotonia and its role in muscle physiology and motor development, including oromotor function and development.
- Study musculoskeletal dysfunction in people with DS, and identify fracture risk factors specific to DS, including the predictive role and value of measures of bone quality/density.
- Evaluate sources of, and potential treatments for, visual acuity defects in people with DS. This activity may include efforts to:
- Evaluate corneal structure in those with DS and determine the integrity of the retinal structure.
- Map the time course for the development of refractive error.
- Evaluate visual neural processing over the course of childhood development.
- Study Obstructive Sleep Apnea (OSA) and other sleep-related disorders (e.g., circadian disturbances, insomnia), the long-term health and metabolic consequences associated with these disorders, and the feasibility and validation of at-home diagnostic tools such as sleep apnea testing, actigraphy, and other wearable technologies; study the efficacy of treatments, such as medications, CPAP, and surgical approaches, including tonsillectomy, adenoidectomy, and hypoglossal nerve stimulator insertion.
- Conduct research on craniofacial growth and upper airway development to help identify types of airway abnormalities in people with DS that may cause aspiration (including microaspiration from reflux), dysphagia, swallowing dysfunction, apnea, and other problems.
- Study pulmonary hypertension in people with DS, including etiology, management, and treatments.
- Examine the impact of dental and oral health/periodontal disease in people with DS on cognition and development, sleep, the immune system, and synergies with common co-occurring conditions, such as potential linkages between hypodontia/microdontia and hypothyroidism.
- Assess the biomechanical and kinematic properties of the vocal tract to develop more complete information on speech physiology in DS. Conduct research on dysmorphologies of the craniofacial and laryngeal structures and motor speech impairments to develop clinical assessments and treatments and improve speech intelligibility.
- Develop preventive measures and treatments to address structural and functional abnormalities in the auditory and vestibular systems of people with DS over the lifespan to optimize hearing and balance.
- Develop intervention strategies using non-pharmacological approaches to manage concurrent co-occurring conditions; such approaches could include technologies to stimulate brain function, dietary interventions to manage type 2 diabetes and similar conditions, and behavioral therapy strategies, such as social engagement, physical activity, educational inclusion, applied behavior analysis, and others to enhance cognition and behavior. Create the evidence base for such interventions, particularly behavior analytic ones, to address domains of development, such as communication, cognition, motor, self-care, and challenging behaviors and to promote inclusion in educational, employment, community, and social settings from infancy through adulthood. Evaluate non-pharmacologic approaches in individuals with DS-AD, for both improving cognitive function and/or preventing cognitive deterioration.
Program Portrait 3: Clinical Research/Co-Occurring Conditions
Congenital Heart Disease (CHD) Research Conducted by INCLUDE Scholars
The Pediatric Heart Network (PHN), sponsored by the National Heart, Lung, and Blood Institute (NHLBI), is helping to achieve a primary goal of the INCLUDE project—fostering future generations of DS researchers. The PHN is a multicenter research enterprise that conducts clinical trials and other clinical research on CHD. Because approximately 50 percent of children with DS are born with CHD, the PHN was a natural home for a program focused on bolstering young investigators interested in pursuing research on DS. With support from the INCLUDE Project in 2019, this NHLBI-led effort conducted a competitive process to fund six INCLUDE Scholars who have conducted research related to DS and the cardiovascular system. Their projects cover a wide age span and include assessment of neurocognitive outcomes, long-term survival, and outcomes of surgery for CHD.
Another project, studying vascular health and risk factors, is premised on the fact that life expectancy among individuals with DS is increasing over historical estimates, and that cardiovascular morbidity and mortality are becoming more common as people with DS get older. The investigators are evaluating risk factors, including obesity, blood lipid abnormalities, and other metabolic issues, for future cardiovascular disease in both children and adolescents with DS. Project researchers will use sophisticated, non-invasive measures of vascular health to compare cardiovascular outcomes of individuals with DS with those who do not have DS. This study recently leveraged funding from the INCLUDE Project to attract additional support.
D. Living and Aging with DS/Services Research
Research studies that benefit the daily lives of people with DS and their families, such as those that inform lifestyle choices and independent living, are a high priority. People with DS are living longer than they were even a few decades ago, and this lengthier lifespan poses many new research questions and opportunities for people with and without the condition. For example, people with DS are at higher risk for developing AD than the general population, and they often develop it at younger ages than those without DS; efforts to discover new treatments for DS-AD may also benefit those with AD who do not have DS.
Enhance Quality of Life
- Conduct research on the efficacy of lifestyle interventions for people with DS across the lifespan to promote healthy behaviors, modulate conditions, such as inflammatory bowel disease or gastroesophageal reflux disease, and/or delay the onset of DS-AD; these approaches may include exercise, diet, dietary supplements, behavioral interventions, and use of technologies.
- Develop applications for mobile devices and computer-based therapies to increase independence for people with DS in activities of daily living, especially self-support technologies, for use in telehealth, home-based, and school settings to improve learning and communication. Develop and/or adapt assistive devices, such as Global Positioning Systems and mobile devices for transportation, or devices that help to facilitate integration of an individual with DS into the workplace, residential or home environment, and community.
- Evaluate the benefits of Augmentative and Alternative Communication to foster communication in people with DS, and develop and validate other tools and interventions aimed at improving language skills and hearing capabilities in those with DS, such as strategies to overcome difficulties in speech intelligibility and literacy.
- Evaluate the benefits of speech supplementation techniques (e.g., gestures, symbols) at different points across the lifespan to foster communicability in people with DS. Identify effective interventions and educational strategies, including the role of learning sign language early in life, to help children with DS process available linguistic input and enhance their communication skills, with the goal of matching children to the therapies best suited to their profiles. Determine the possible influences of race, ethnicity, and culture on language development in children with DS.
- Continue to conduct research on optimal educational methods for children with DS, mechanisms to support the transition from high school to adulthood, and development of functional and job skills, with the recognition that education, literacy, and academics facilitate success in post-secondary education and employment.
- Examine cohorts of younger to older age adults with DS to develop a model of life-stage transitions among adults to aid with planning for changes in autonomy, employment, retirement, and social and family engagement.
- Identify factors (i.e., medical, intellectual, social, familial) that may be protective for fostering maximal independence and community inclusion, with a specific focus on individuals with DS who are aging in non-disability community settings for seniors. Study what measurable skills, such as self-management skills for co-occurring conditions, are meaningful to enhancing quality of life and promoting independence among people with DS. Such work may include studies of:
- Comparative models of care to explore support factors and mitigation strategies to identify best practices in supporting adults with DS experiencing mild cognitive impairment or in the early stages of dementia
- Current practices of supporting adults with advanced dementia and comparative studies of which models and practices best mitigate advanced-stage-dementia related pain, decline, loss of function, and medical conditions and provide for the highest degree of comfort and quality of care
- Investigate the impact on families of caring for individuals with DS as they age, and as overall lifespans of those with DS continue to increase. Such work may include the following:
- Identifying the factors that lead to effective functioning or challenges in families that include an individual with DS
- Understanding the impact on the family, including the individual with DS, as that person leaves the school system
- Researching the physical and mental health and lifespans of the parents, siblings, and other caregivers, as well as the effectiveness and validity of support-staging models of decision-making among caregivers of adults with DS-AD with application to family counseling and design of services
- Examining the personal and social support networks of middle-age and older adults with DS and the elements of these networks that contribute to continued function, autonomy, and quality of life
- Study the impact of behavior problems and psychiatric disorders on the daily functioning, socialization, academics, and quality of life of people with DS.
- Develop tools to foster coping skills among people with DS during periods of grief/loss and disruption of routine, including accessible materials and other resources for managing depression and anxiety.
- Use lessons learned from families’ experiences with the SARS-COV-2 pandemic to develop strategies that include people with DS in planning for future public health and disaster preparedness efforts, such as maintaining caregiver access to individuals with DS who may be isolated in the hospital.
Increase Inclusion of People with DS in Research Across the Lifespan
- Take into account, when designing specific research studies, how potential participants view themselves (including identities of race, ethnicity, gender, class, and sexual orientation) and, to the extent feasible, recruit diverse populations of people with DS across the lifespan into research studies.
- Develop research study materials that are accessible to individuals with DS, including study descriptions, informed consent/assent documents/methods, and information on confidentiality and privacy of data. Engage people with DS and their caregivers in study design to increase the appropriateness of these materials and ensure that the presentation of research topics and results does not unintentionally cause psychological stress in potential participants.
- Encourage researchers to participate in DS-related outreach efforts to share the latest information and help inform individuals with DS and their families about research progress, thus encouraging additional participation in studies. Foster additional efforts to educate caregivers of people with DS about the value of participating in research.
- Working with the DS Consortium and DS-Connect® team, explore a variety of dissemination methods for reaching healthcare providers with information about recent research findings in DS. In particular, develop and disseminate evidence-based educational materials regarding management of co-occurring conditions in DS. Encourage NIH to incorporate people with DS in its overall health education efforts.
- Consider mapping research studies to the National Institute on Minority Health and Health Disparities Research Framework to ensure appropriate inclusion of the effects of social determinants of health.
- Study the cross-cultural and linguistically diverse needs of people with DS and apply the findings to education and recruitment efforts to ensure equitable access and optimize retention. Develop and promote interventions that are culturally responsive to the needs of diverse individuals and groups.
Expand Knowledge on DS, Aging, and DS-AD
- Study whether aging among those with DS has a greater impact on physiologic and cognitive processes than it does for those without DS. Efforts could include studies of the:
- Factors that affect the risk of dementia
- Differential impact of aging on organ systems in people with DS, such as changes in bone mass and chronic inflammatory conditions
- Support research on variations in aging patterns, including consideration of lifestyle factors, among subpopulations of people with DS.
- Explore potential protective factors for age-related dementia, including complementary and integrative health approaches, cognitive stimulation and social engagement, exercise and weight management, and nutrition and dietary practices.
- Study the specific impact of postmenopausal hormone replacement therapy (HRT) use by women with DS to determine if it reduces the cumulative risk for DS-AD, and if so, identify the optimal time and duration for postmenopausal HRT use in this population.
- Study how the aging process, dual diagnosis of DS and another condition (such as ASD), or mosaicism affects the progression of chronic conditions or infection.
- Explore the impact of having type 2 diabetes on the development of DS-AD.
- Study the relationship between changes in sleep, behavior, cognition, and biomarkers for DS-AD.
- Examine the impact of caring for people with DS as they age by considering the needs of caregivers in study design. Study the health impact on individuals with DS if their caregiver has a significant health issue or dies.
- Study long-term care options and end-of-life decision-making for older individuals with DS.
Program Portrait 4: Living and Aging with DS
Alzheimer’s Biomarker Consortium-Down Syndrome (ABC-DS) Project
Adults with DS are at high risk for developing AD. Virtually all adults with DS have neuropathological changes consistent with AD by age 40, including deposits of amyloid-beta (Aβ) in diffuse and neuritic plaques, and most will develop clinical dementia by their late 60s. The high risk for DS-AD has been attributed, at least in part, to triplication and overexpression of the gene for APP on chromosome 21, leading to elevated levels of Aβ peptides. The wide variation in age at onset of dementia among those with DS, ranging from younger than 40 years to older than 70 years of age, suggests that additional genetic, biological, and environmental factors modify the rate and degree of Aβ deposition or clearance, and that these factors may be important modifiers of risk, accelerating or slowing disease progression. Development of empirically supported methods for early diagnosis of dementia in DS, biological characterization of the preclinical and early phases of DS-AD, and identification of risk factors for AD progression are critical to the early diagnosis of dementia and for the development of effective interventions and treatments.
ABC-DS is a multidisciplinary, multisite longitudinal study examining biomarkers of DS-AD in a large cohort of adults with DS, age 25 and older. The National Institute on Aging (NIA) and the NICHD initiated ABC-DS in 2015 by funding two groups of research collaborators—Neurodegeneration in Aging Down Syndrome (NiAD, U01AG051406) and Alzheimer’s Disease in Down Syndrome (ADDS, U01AG051412). In September 2020, the continuation of ABC-DS was funded by the NIA, NICHD, and the INCLUDE Project (U19AG068054) as one combined study.
ABC-DS researchers will follow the cohort of people with DS to conduct three projects:
- Investigate how DS-AD parallels and differs from sporadic AD within an amyloid, tau, neurodegeneration framework, and identify modifiers of risk of conversion/progression.
- Identify genetic modifiers of the development of DS-AD.
- Translate outcomes to a precision medicine framework and expedite clinical trials.
Importantly, the next iteration of ABC-DS includes an emphasis on increasing the diversity of individuals in the cohort of adults with DS. The AD/DS Outreach, Recruitment, and Engagement Core will help rapidly disseminate information to DS communities and engage underrepresented groups.
E. Research Infrastructure and Tools
Diagnostic and screening measures used for DS and related conditions have continued to evolve in recent years. However, utilization of more specialized measures of function across domains could facilitate more refined phenotyping and identification of biomarkers for medical, cognitive, and behavioral features related to DS.
In the near term, the scientific community needs to further improve tools, techniques, methods, and measures to move toward a minimum set of common measures for use across studies, age groups, and developmental and behavioral domains. The field may benefit from a consensus on common domains and on a core set of standardized tests and measures for use in clinical research on DS to allow for comparability across studies, noting that domains appropriate for one stage of life may not be appropriate for others. In addition, making common research resources available to researchers, such as new models for DS, research infrastructure, and data and tissue repositories, will allow research to move forward more rapidly.
Expand Research Tools
- Develop additional new model systems for studying DS at the cellular, organ (in addition to brain), and genetic levels.
- Study the effects of perturbation of individual chromosome 21 genes on the differentiation and maturation of neurons, glia, and synapses in brain organoids, as well as in model organisms such as C. elegans and Drosophila.
- Develop and support new animal (i.e., mouse, rat, or NHP) models for conducting preclinical research on DS, including testing pharmacological and genetic interventions, and conducting anatomical and behavioral analyses of brain development. NHP models, such as marmosets, have the potential to shed light on social behaviors, cognition, and communication that murine models cannot replicate. Prioritize the development of models that minimize changes to non-chromosome 21-equivalent genes, and those that can reflect the structural changes in the human brain and immune system without introducing extraneous genetic material.
- Develop and support new human cellular/organoid cultures for conducting preclinical research on DS.
- Design new treatment paradigms and pathways for testing pharmaceuticals in DS mouse models (specifically, dose-response and toxicity studies).
- Develop nanotechnology and other small-molecule approaches to enhance contrast of amyloid imaging reagents for finer resolution studies in younger individuals with DS.
- Develop human DS cellular models (e.g., iPSCs differentiated into neuronal cultures) to study variations by sex and ancestry.
- Use both in vivo and in vitro model systems to study cardiovascular function and therapy response.
- Refine outcome measures that are already validated in people with DS, and disseminate these outcome measures to the research community. Emphasize measures that have demonstrable clinical utility, such as identifying changes in language, behavior, cognition, or adaptive skills. Build on the NIH Toolbox Cognitive Battery to develop or adapt additional outcome measures for studying people with DS who are low functioning, very young, or adolescents. Track outcomes during early development to allow evaluation of the impact of interventions at different life stages.
- Link cognitive phenotypes of DS to validated developmental measures, including speech and language, auditory function, behavioral, and psychological abnormalities. Use Magnetic Resonance Imaging (MRI), functional MRI (fMRI), diffusion-tensor imaging (DTI), and other emerging imaging modalities in conjunction with specific neurocognitive assessment measurements to examine major pathways and determine how those pathways differ in persons with DS. For example, this research could address the correlation among cognitive function/language impairment/behavior issues in individuals with DS and co-occurring ASD.
- Develop biomarkers and other assessment tools to diagnose and analyze developmental delays and cognitive impairments (including dementia) that also permit tracking the effectiveness of early interventions. Specifically, identify the clinical, cognitive, genetic, and biochemical biomarkers of DS-AD for use in detection and management of disease progression. Develop or improve methods to detect mild cognitive impairment in DS to aid in the early diagnosis of DS-AD. Validate these tools for use in clinical settings.
- Develop diagnostic/screening tools and biomarkers for autoimmune conditions in people with DS, including celiac disease and arthropathy, prior to the development of symptoms.
- Assess how asthma diagnostic criteria and screening tools should be applied to individuals with DS.
- Develop screening tools and biomarkers for infectious diseases that occur more commonly in people with DS (e.g., pneumonia).
- Conduct research to identify new biomarkers for hypothyroidism in addition to antithyroid antibodies in people with DS.
- Develop screening tools for depression, anxiety, and other co-occurring mental health conditions in people with DS.
- Develop diagnostic and screening tools for hematologic disorders in people with DS to permit tailored treatments.
- Refine the diagnostic and screening tools for vision-related conditions in people with DS.
- Develop or improve methods to assess auditory and vestibular function over the lifespan of people with DS for use in screening during routine health examinations.
- Refine the diagnostic and screening tools for type 1 diabetes in people with DS.
- Assess the value of and develop additional screening tools and technologies (such as wearables) for OSA in people with DS to improve diagnosis without the necessity of sleep studies in medical facilities.
- Facilitate collaboration between neuropathologists and DS clinicians to assess the usefulness of current model systems and biomarkers for DS neurobiology.
- Develop functional intervention models that address behavioral and psychological symptoms. Use neurocognitive tools and brain imaging technologies (i.e., MRI, fMRI, DTI, electroencephalogram) to link neurocognitive performance and health status in people with DS with underlying brain structure.
Improve Research Infrastructure
- Increase public awareness of and registration in DS-Connect®: The DS Registry. Relay personal experiences from the DS community, such as through videos and other outreach methods describing why individuals have chosen to participate in research, and explaining how research has impacted their lives.
- Set up a family-to-family outreach effort allowing families who are already enrolled in the DS-Connect® registry to explain to others why they joined and raise awareness about opportunities to participate in research.
- Ensure that participants receive the overall study results from any research projects in which they participated, in accessible language.
- Expand the DS-Connect® website to promote non-DS-Connect events and articles. Expand and update the DS-Connect® and/or the NIH DS websites with listings of upcoming clinical trials and treatment guidelines.
- Work with the Centers for Medicare and Medicaid Services to provide information and materials about the DS-Connect® registry and upcoming research studies that are seeking participants from healthcare organizations that accept Medicaid.
- Work with DS organizations and experienced clinical trial specialists to create accessible and appropriate recruitment materials for DS studies, using language that is easily understandable to people with DS and their families; consider both visual and non-visual materials.
- Study how health care practice may best foster engagement and participation of people with DS in research. Identify ways to foster community-engaged research, collaborating when possible with people with DS, caregivers/supporters, and community partners; use community advisory boards to augment ethical reviews of research by institutional review boards.
- Augment systems for sharing data from published cohorts and make results available in a searchable format, including fostering international data sharing. Establish a publicly available, centralized repository for DS data, either through or in conjunction with the DS-Connect® registry and the INCLUDE Data Coordinating Center, so that researchers may compare DS-specific data with data on the general population, people with intellectual and developmental disabilities other than DS, siblings of people with DS, and people with AD. Use common datasets and Common Data Elements to ensure standardized collection of phenotypic, clinical, and ‘omics data. Develop training and other support for DS clinics to support digitization of clinical data for submission to a centralized repository/database, and encourage the use of global identifiers that allow data sharing between databases without revealing personally identifiable information.
- Through the INCLUDE Data Coordinating Center, create a large cohort study of individuals with DS across the lifespan to accelerate research into co-occurring conditions. Provide researchers and the broader DS community with access to the cohort data and data mining and analysis tools, and facilitate data sharing and linkages of datasets using unique identifiers that preserve individual confidentiality. Ensure full data sharing with appropriate privacy protections and adherence to the “FAIR” principles (Findable, Accessible, Interoperable, and Reusable) per NIH Data Commons guidelines.
- Expand the research infrastructure for DS by establishing or augmenting collaborations among existing clinical sites and research networks at medical/academic institutions that already conduct research related to DS and its co-occurring conditions. Encourage this federation of sites to conduct large studies, such as a longitudinal cohort study or multisite clinical trials. To facilitate the translation of basic and translational research to clinical practice, such sites could:
- Support an interdisciplinary team of researchers and clinicians, including the development of new researchers in DS, some of whom may conduct implementation science projects to ensure that the underlying research results benefit the DS community.
- Encourage non-DS focused basic scientists, research pediatricians, and other medical specialists with experience studying co-occurring conditions to expand their focus to include specific investigations in DS.
- Facilitate enrollment of condition-specific subgroups, age ranges, or underrepresented populations of people with DS into research studies.
- Develop a range of trial designs to enhance reproducibility of data in the DS population, for which sample size may be limited.
- Establish a federation of biorepositories that will permit biobanking of cells, plasma, serum, CSF, and brain and other tissues for research purposes,[14] including samples from individuals with cancer with DS. Integrate biorepository data with the DS-Connect® registry and the INCLUDE Data Coordinating Center as feasible, including use of minimal common datasets to ensure standardized collection of phenotypic information. Standardize sample collection and processing methodologies and policies for consistent, equitable sample distribution, and establish review and distribution processes for researcher access to the samples/data. Identify and address barriers and motivating factors to donation. Consideration should also be given to:
- Linking the DS repository with the NIH NeuroBioBank and the existing ADRC Brain Banks, so that tissue from people with DS can be compared to those obtained from individuals with AD and other disorders
- Collecting neurotypical control samples
- Expand federally funded research training programs to ensure a vibrant pipeline of researchers doing work in DS, and host scientific workshops that bring emerging investigators together with established scientists in the field for training in clinical trials.
Program Portrait 5: Research Infrastructure and Tools
Using the Pediatric Trials Network (PTN) to Test Therapeutics in Children with DS
Only a small percentage of drugs and devices approved by the FDA have been labeled for pediatric use. NICHD established the PTN in 2010 to conduct clinical research and collect data to assist the FDA in revising medication labels for safer and more effective use in children. Working with research sites around the country, the PTN studies the formulation, dosing, efficacy, and safety of drugs, as well as medical devices, for use in children. The structure allows the network to address many of the challenges related to conducting clinical trials in children, such as having a limited number of subjects at one site, competing research priorities, and a lack of trained investigators.
Recently, NICHD funded an expansion of the PTN’s trial structure to develop prospective trials to assess the safety and efficacy of therapeutics prescribed for children with DS. The effort—called the PTN PK, PD, and Safety Profile of Understudied Drugs Administered to Children per Standard of Care—will train investigators at a core set of sites on clinical pharmacology-based research and clinical trials in DS to evaluate the PK/PD of drugs administered to children with DS as part of the standard of care. This approach will allow the collection of data in a real-world setting, allowing researchers to understand differences in how children with DS may metabolize drugs, and to evaluate the influence of genetic factors on drug metabolism and efficacy.
In addition, the PTN is conducting a study in children with DS and with the co-occurring condition, ADHD, called the Guanfacine for Hyperactivity in Children with DS study. Millions of children are affected by ADHD, which is often associated with behavioral problems, learning disabilities, psychiatric conditions, such as depression, and increased risk of injury. However, FDA-approved treatment options for ADHD have been studied almost exclusively in typically developing children. Moreover, clinicians may be using these medications for treatment in DS, but with no data to drive their dosing decisions. Guanfacine is one of the most commonly used medications for treating ADHD, but no PK/PD data exist for its use in children with DS. This prospective, randomized, placebo-controlled trial, in children with DS ages 6 to 12 years, will provide the data needed to determine the safety and efficacy of the treatment in this specific population.
Conclusion: Emerging Research Opportunities
The field of DS research has undergone some remarkable changes since the last NIH research plan was published in 2014. In that research plan, Down Syndrome Directions, the research objectives were significantly expanded, in comparison to the first DS-specific plan published in 2007, to create a more balanced perspective on the health needs and multiple co-occurring conditions of DS beyond intellectual disability, including the addition of research on DS and aging. Although not all of the 2014 plan’s objectives have been met, researchers and the DS community have made significant progress in DS-related research. For example:
- The development of iPSC and cerebral organoid culture systems and other basic science advances are providing new tools to probe early neurodevelopment; the availability of rapid, efficient gene-editing tools, such as CRISPR/Cas9, have revolutionized researchers’ ability to engineer cellular and animal models.
- Although a few significant, single genes on chromosome 21 are still the subject of intense scrutiny, newer studies take a more nuanced view on the impact of multiple genes across the entire chromosome, as well as the role of genes on other chromosomes and even environmental factors; in fact, many of these studies are incorporating ‘omics technologies to support a systems-biology approach that was not feasible a decade ago.
- Recognition of DS as an “interferonopathy” due to altered immune system regulation is beginning to inform a more complete model of the interplay between the immune system, oxidative stress, bioenergetics, and neurogenesis on cognition and many other aspects of DS.
- Several large cohort studies have provided a better understanding of the pathophysiology of DS-AD (PMID: 30733618), but more recent recognition of a worrisome “regression” phenotype reminds us of how much we have yet to learn about some of the neurological conditions that co-occur with DS.
- The paucity of medication trials tailored to people with DS (with the exception of several exploring the optimal chemotherapy for childhood leukemia in DS, and some failed trials to improve cognition or even prevent dementia) (PMID: 28884975; PMID: 24573065) is improving, particularly with support from the INCLUDE Project.
The impact of the INCLUDE Project should not be underestimated; it has infused the field with new funding, brought new investigators into DS research, and encouraged new and “out-of-the-box” approaches to this well-known chromosomal disorder, fundamentally changing the culture of DS research conducted and supported by NIH. The emphasis on support of trainees and junior faculty engaging in DS-related research, through institutional training grant supplements, Clinical and Translational Science Awards training supplements, the PHN Scholars program (see Program Portrait 3), and individual fellowship and career development awards, is resulting in new and younger scientists joining the DS research community. The additional focus on transformative research is also encouraging new and established investigators to explore exciting areas of basic science inquiry. All of these measures increase the pool of investigators involved in DS research and fulfill the congressional mandate to “expand the current pipeline of DS research” (see Appendix E: Congressional Directives on DS Research).
Despite the INCLUDE Project’s recent launch, with the first supplements funded a short time ago, it has still contributed to several specific outcomes and discoveries, as noted in this research plan. In addition, some of the promising DS projects funded through INCLUDE and other NIH sources allow identification of aspirational scientific goals that may lead to exciting discoveries in the future.
One such aspirational goal is the development and expanded availability of improved rodent models for DS. Another aspirational goal focuses on advancing prenatal treatments to prevent certain aspects of DS, such as cognitive impairment (PMID 33098770), immune disorders, or AD; while more preclinical studies are needed prior to engaging in human trials, the possibilities are intriguing. The concept that an extra copy of a chromosome could be selectively “turned off” or “silenced” in a cell was only recently achieved in a cell culture environment (PMID: 30518921); testing this chromosome silencing in a mouse model of DS to prevent amyloid plaque deposition in the brain and onset of dementia symptoms remains as an aspirational goal that could be a breakthrough not only in the field of DS research, but also for many other conditions.
Community input continues to be a critical aspect of improving treatments for some of the most challenging aspects of DS. Parents often report that poor communication and speech articulation, as well as poor sleep quality, have a major impact not only on the well-being of the person with DS, but also on other family members. The possibility of developmental regression in teens and young adults with DS, and the onset of dementia as people with DS age looms for many families. Developing clinical trials to improve understanding of the causes and range of clinical presentations specifically in people with DS requires consistent and frank engagement between the DS community and researchers, including those who study conditions other than DS. For example, findings from an AD prevention trial that uses an anti-amyloid therapy are of interest within the DS community and the non-DS community alike.
The unique challenges posed by the COVID-19 pandemic also provide opportunities, such as understanding the heightened risk factors for more severe outcomes in those with DS infected with the SARS-CoV-2 virus. Through supplemental awards and other mechanisms, investigators can learn about the roles played by immune factors in COVID-19 infection, which in turn may help understand risks and resiliencies in in both the DS and general population. The knowledge gained will help all of us prepare for the next pandemic or other emerging health threats that may have a disproportionately negative impact on those with DS.
Perhaps the most important outcome of the previous research plan is the enhanced engagement and partnership with and within the DS community. The NIH commitment to research participation by individuals across the lifespan, including those with intellectual disabilities and DS (PMID: 29285540), is changing the clinical research landscape. All NIH workshops hosted since 2019 (see Appendix D: DS-Research Related Meetings Since 2014) have included a voice-of-the-participant, parent, and/or self-advocate perspective in their speaker rosters. These presentations are among the most dynamic and provocative and serve as touchpoints for subsequent discussions.
Inviting a wider range of individuals to engage in clinical research—both as participants and as clinicians leading the studies—is now a cornerstone of NIH efforts, including the PTN studies to understand drug metabolism in children with DS who are already taking medications, and the standalone trial of guanfacine in children with DS and ADHD (see Program Portrait 4). Developing a cadre of investigators and clinical trialists who understand the unique needs of the DS population, can develop relevant therapies, and are comfortable proposing new clinical trials to test the therapies in this population is an important step in the inclusion process. Likewise, the more recent emphasis on developing outcome measures and biomarkers to serve as endpoints for clinical trials is paving the way for future trials of interventions for a full range of co-occurring conditions of DS. These efforts underscore the importance of diversity, equity, inclusion, and accessibility in our workforce and in the research participants recruited for DS studies.
Appendices
- Appendix A: NIH-Led DS Groups
- Appendix B: Input into Development of the Revised Plan
- Appendix C: INCLUDE Funding Opportunity Announcements
- Appendix D: DS-Research Related Meetings Since 2014
- Appendix E: Congressional Directives on DS Research
- Appendix F: Training in DS Research
- Appendix G: Bibliography
[1] Could include studies of AD, dementia, ASD, anxiety, ADHD, depression, bipolar disorder, post-traumatic stress disorder, schizophrenia, obsessive-compulsive disorder, Parkinson’s disease, traumatic brain injury, cerebral palsy, stroke, movement disorder/restless leg syndrome, Moyamoya disease, regression, seizure disorders/infantile spasms/epilepsy, and autoimmune encephalitis.
[2] Could include studies of CHD, heart arrhythmias, hypertension, cardiomyopathy, high cholesterol, atherosclerosis, atherosclerotic and non-atherosclerotic cardiac ischemia, peripheral artery disease, and myocardial infarction.
[3] Could include studies of hypothyroidism, hyperthyroidism, Grave’s disease, and Hashimoto’s disease.
[4] Could include studies of asthma, reactive airway disease, pulmonary hypertension, and pneumonia.
[5] Could include studies of amblyopia, astigmatism, cataracts, glaucoma, hyperopia, keratoconus, myopia, nystagmus, strabismus, and blocked nasolacrimal duct.
[6] Could include studies of eustachian tube dysfunction, laryngomalacia, chronic rhinitis, hearing loss, deafness, macroglossia, obstructive sleep apnea, sinusitis, and upper respiratory infection.
[7] Could include studies of acute T-cell lymphoid leukemia, acute B-cell lymphoid leukemia, acute myeloid leukemia, chronic lymphocytic leukemia, chronic myeloid leukemia, Transient Myeloproliferative Disorder, and Transient Abnormal Myelopoiesis.
[8] Could include studies of gastroesophageal reflux, chronic constipation, chronic diarrhea, dysphagia, celiac disease, Hirschsprung disease, pyloric stenosis, irritable bowel syndrome, inflammatory bowel disease, peptic ulcers, gallstones, hemorrhoids, diverticulitis, duodenal atresia, stenosis or web, anal stenosis or atresia, esophageal atresia, dysuria, voiding dysfunction, kidney disease, cystic dysplastic kidney, hydronephrosis, hydroureter, posterior or anterior urethral valves, renal agenesis, vesicoureteral reflux, and nonalcoholic fatty liver disease.
[9] Could include studies of acne, alopecia areata, atopic dermatitis/eczema, boils/hidradenitis suppurativa/folliculitis, cellulitis, psoriasis, rosacea, tinea capitis, fungus, vitiligo, and xerosis (dry skin).
[10] Could include studies of arthropathy, hypotonia, atlantoaxial instability, fractures, cervical spine degeneration, osteopenia, osteoporosis, osteoarthritis, and scoliosis (curvature).
[11] Could include studies of congenital/infant diabetes, insulin resistance, and type 1, type 2, and pre-diabetes.
[12] Could include, but not limited to, studies of type 1 diabetes, celiac disease, Hashimoto’s thyroiditis, alopecia areata, atopic dermatitis/eczema, dermatitis herpetiformis, dermatomyositis, hidradenitis suppurativa, lichen planus, lichen sclerosis, vitiligo, psoriasis, psoriatic arthritis, arthropathy, rheumatoid arthritis, vasculitis, hemolytic anemia, thrombocytopenic purpura, myositis, restless leg syndrome (rarely autoimmune), Meniere’s disease, autoimmune encephalitis, inflammatory bowel disease/Crohn’s disease, narcolepsy, Kawasaki disease, Pediatric Autoimmune Neuropsychiatric Disorders Associated with Streptococcal Infections syndrome, sarcoidosis, and systemic lupus erythematosus.
[13] Could include, but not limited to, studies of group A streptococcus, C. difficile infection, recurrent otitis media, recurrent sinusitis, RSV, pneumonia, candidiasis, croup, chronic urinary tract infection, impetigo, cellulitis, Staphylococcus (Staph) infection, cold sores/human papilloma virus, shingles, periodontitis, gout, sepsis, tuberculosis (TB) or latent TB, SARS-CoV-2, and upper respiratory infections.
[14] Biospecimens could include, but are not limited to, buccal DNA, hair, blood, cord blood, brain, CSF, saliva, tissues from surgeries, urine, stool, skin, amniotic fluid, placenta, and dried bloodspots collected during newborn screening.
This page last reviewed on March 29, 2024
