You are here
April 5, 2022
Compound blocks excess mucus secretion in mouse lungs
At a Glance
- In mice, a compound called SP9 blocked the excess secretion of mucus, a feature of many lung diseases that can cause difficulty breathing and other symptoms.
- The compound has the potential to be developed into a drug to treat mucus accumulation in many common lung diseases.
Mucus plays a vital role in lung health. It serves as a lubricant to keep tissues from drying out. It helps filter out dust, allergens, and harmful microorganisms. But excess mucus production followed by rapid secretion (called mucus hypersecretion) can clog the airways and make it hard to breathe. Mucus hypersecretion is a hallmark of many serious lung diseases, including asthma, chronic obstructive pulmonary disease (COPD), and cystic fibrosis.
Drugs developed to treat some of these conditions can reduce inflammation, expand the airways, or thin the mucus, which can help people breathe. But no treatments stop rapid mucus secretion.
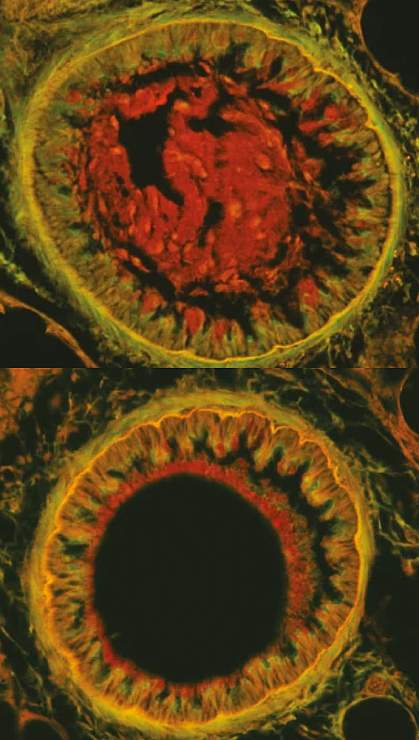
An international team of researchers has been studying ways to slow the release of mucin, a key component of mucus. Mucins are found within molecular packets, called secretory granules, in the epithelial cells that line the lungs. In response to a signal in the cell, these granules fuse with the cell membranes to release mucin into the airways. There, mucin interacts with water and salts to create mucus. If too much mucin is released too quickly, it can overwhelm the available water. This produces mucus that is too thick and clogs airways.
The team focused on blocking a protein called synaptotagmin-2, or Syt2. Syt2 is found on the surface of the granules containing mucin. Fusion of these granules with the cell membrane depends on Syt2 interacting with proteins in the cell membrane.
In their new study, the researchers created a peptide—a short chain of amino acids—called SP9 to block Syt2. Peptides often have unstable structures. To make SP9, the team used a technique called hydrocarbon stapling to freeze it in a shape that blocks Syt2 from interacting with the cell membrane proteins.
The work was supported by NIH’s National Heart, Lung, and Blood Institute (NHLBI), National Institute of Mental Health (NIMH), and National Institute of Allergy and Infectious Diseases (NIAID). Results were published on March 23, 2022, in Nature.
In lab testing, SP9 shut down the membrane fusion process by attaching to Syt2. The researchers next tested SP9 in human airway cells grown in the lab. With a special carrier section added to its sequence, the peptide successfully entered the cells. When the cells were stimulated to secrete mucin, SP9 reduced secretion by 83%.
Next, the team tested SP9 with the carrier in living mice by spraying it directly into the animals’ lungs. Imaging showed that around three-quarters of epithelial cells took up the peptide. SP9 reduced mucin secretion by around 80% and mucus accumulation in the airways by a third. Notably, it didn’t interfere with the normal, slower mechanism that secretes a low level of mucin constantly to protect the lungs.
“An inhaled drug like this could help someone during an acute attack of airway disease by stopping the rapid secretion of mucin,” says Dr. Burton Dickey from the University of Texas MD Anderson Cancer Center, one of the study’s leaders. “It might also improve airway function in some patients if administered chronically.”
Further improvements are needed to turn SP9 into a drug that could be delivered into human lungs and tested in people.
—by Sharon Reynolds
Related Links
- “Sweat Sticker” for Diagnosing Cystic Fibrosis
- Experimental Treatment Helps Patients Hospitalized with COPD
- Replacing Function of Impaired Cystic Fibrosis Protein
- Controlling Childhood Asthma
- How Cystic Fibrosis Promotes Lung Infections
- Marvels of Mucus and Phlegm
- Cystic Fibrosis
- Chronic Obstructive Pulmonary Disease (COPD)
- Asthma
References: Inhibition of calcium-triggered secretion by hydrocarbon-stapled peptides. Lai Y, Fois G, Flores JR, Tuvim MJ, Zhou Q, Yang K, Leitz J, Peters J, Zhang Y, Pfuetzner RA, Esquivies L, Jones P, Frick M, Dickey BF, Brunger AT. Nature. 2022 Mar 23. doi: 10.1038/s41586-022-04543-1. Online ahead of print. PMID: 35322233.
Funding: NIH’s National Heart, Lung, and Blood Institute (NHLBI), National Institute of Mental Health (NIMH), and National Institute of Allergy and Infectious Diseases (NIAID); Deutsche Forschungsgemeinschaft; Cystic Fibrosis Foundation.
