You are here
June 13, 2017
A noninvasive deep brain stimulation technique
At a Glance
- Researchers designed a noninvasive way to stimulate cells deep in the brains of mice without affecting surrounding tissue.
- The results suggest a more convenient strategy for treating Parkinson’s disease and mental health disorders using electrical stimulation.
Brain stimulation therapies can play a role in treating certain mental health disorders. The approaches involve activating or inhibiting brain activity using electricity. Deep brain stimulation was first developed as a treatment for Parkinson’s disease and subsequently used to treat epilepsy. It has since been studied as a treatment for various mental health issues, including treatment-resistant depression and obsessive compulsive disorder.
In deep brain stimulation, a pair of electrodes is implanted in the brain and controlled by a generator implanted in the chest. Stimulation is continuous, and its frequency and level are customized to the individual. However, deep brain stimulation requires brain surgery. That makes it a higher risk option than other treatments.
To explore noninvasive deep brain stimulation techniques, a team led by Dr. Ed Boyden at the Massachusetts Institute of Technology tested strategies for delivering electrical stimulation to different brain areas in mice. The study was funded by NIH’s National Institute of Neurological Disease and Stroke (NINDS), National Institute of Mental Health (NIMH), and others. Results were published on June 1, 2017, in Cell.
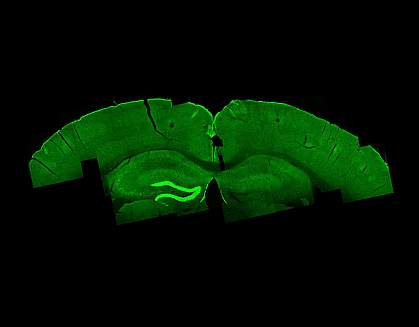
The scientists delivered electrical current into the mouse brain using electrodes placed on two different locations of the scalp. Each electrode delivered a different high frequency current that most brain cells don’t respond to. When the two currents collided deep inside the brain, they generated a lower frequency that neurons do respond to and thus affected the cells’ activity. This technique is called temporal interference stimulation.
The team measured the neuronal firing frequency in the hippocampus while delivering different electrical currents. They found different combinations of frequencies that could be used to alter cell firing rates. By narrowing or widening the placement of the electrodes, the team could direct the current to target the precise brain region they wanted to activate. Using this strategy, the team directed current at different regions of the motor cortex and found that they could evoke movement of different body parts, including the whiskers and forepaws.
The researchers investigated the safety of the stimulation by tracking tissue temperatures, looking for signs of DNA damage and cell death, and assessing seizure activity. The technique didn’t compromise the brain tissue, alter the temperature beyond normal ranges, or induce seizures. With further development, temporal interference might be tested for its ability to stimulate neurons deep in the human brain.
“With the ability to stimulate brain structures noninvasively, we hope that we may help discover new targets for treating brain disorders,” says the paper’s lead author, Dr. Nir Grossman, who is now at Imperial College London.
“People have used non-invasive brain stimulation to study a wide variety of phenomena, from mood to memory to driving ability to trust,” Boyden says. “Now, we can do these types of studies, hopefully, in deeper targets in the brain.”
—by Tianna Hicklin, Ph.D.
Related Links
- Deep Brain Stimulation Curbs Parkinson Symptoms
- Parkinson’s Disease: Understanding a Complicated Condition
- Brain Stimulation Therapies
- Deep Brain Stimulation for Parkinson's Disease
- Depression
- Obsessive-Compulsive Disorder
- Epilepsy Information Page
- Brain Basics
References: Noninvasive Deep Brain Stimulation via Temporally Interfering Electric Fields. Grossman N, Bono D, Dedic N, Kodandaramaiah SB, Rudenko A, Suk HJ, Cassara AM, Neufeld E, Kuster N, Tsai LH, Pascual-Leone A, Boyden ES. Cell. 2017 Jun 1;169(6):1029-1041.e16. doi: 10.1016/j.cell.2017.05.024. PMID: 28575667.
Funding: NIH’s National Institute of Neurological Disease and Stroke (NINDS), National Institute of Mental Health (NIMH), National Center for Advancing Translational Sciences (NCATS), National Institute on Aging (NIA), National Center for Research Resources (NCRR), and Eunice Kennedy Shriver National Institute of Child Health and Human Development (NICHD); New York Stem Cell Foundation; Massachusetts Institute of Technology; National Science Foundation; Jeremy and Joyce Wertheimer; Google; the Wellcome Trust; Belfer Neurodegeneration Consortium; Glenn Foundation for Aging Research; Alana Foundation; Cure Alzheimer's Fund; JBP Foundation; Brain & Behavior Research Foundation; Sidney R. Baer Jr. Foundation; and Harvard University.
