You are here
February 13, 2018
Injection prompts mouse immune system to destroy tumors
At a Glance
- In studies using mouse models, scientists found a combination of agents that, when injected into a tumor, directs the immune system to destroy not only the injected tumor, but tumors of the same type throughout the body.
- This tumor vaccination approach doesn’t depend on knowing the unique characteristics of a tumor, so it could in theory be applied to many forms of cancer.
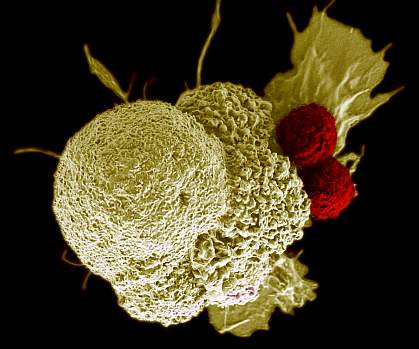
All malignant tumors harbor genetic alterations. Some of these mutations lead to the production of modified proteins that can trigger an immune response. Tumors are often infiltrated by immune cells called T cells that recognize these altered proteins, or antigens. The field of cancer immunology aims to harness these immune responses. Several new methods of treating cancer, called immunotherapies, have been developed. These approaches, however, can be lengthy and costly, and have serious side effects.
A research team led by Dr. Ronald Levy at Stanford University aimed to develop a way to stimulate immune cells in the tumor to mount a stronger response to the cancer cell antigens around them—essentially, a cancer vaccination. They screened for compounds that could be injected into tumors in minute amounts and prompt a strong immune response. By using agents at very low doses, they reasoned, the approach should minimize any potential side effects. The work was funded in part by NIH’s National Cancer Institute (NCI). Results were published on January 31, 2018, in Science Translational Medicine.
The team screened a series of immune-activating molecules. They also tested antibodies that block the activity of immune cell checkpoint proteins, which normally keep immune responses in check to prevent damage to normal cells. Past studies have shown that tumors often commandeer these proteins to suppress immune responses against them.
An immune-activating molecule called CpG and an antibody called anti-OX40 proved to be the most potent pair. This combination proved effective in mouse models of several cancers, including lymphoma, breast cancer, colon cancer, and melanoma.
While the injections into the tumors involved minute quantities of the molecules, the vaccinations prompted system-wide responses. Mice with two tumors of the same type in different locations had both tumors disappear. The distant tumors rarely recurred (in 3 of 90 mice), and these tumors were sensitive to a second injection of CpG and anti-OX40.
Mice successfully treated by the vaccinations weren’t immune to tumors of other types. This shows that the vaccinations work by triggering a specific immune response within the injected site. To see whether the approach could work against complex tumors, the scientists tested mice who had a mixture of different tumor cells at one site. The vaccination induced immune responses against both types of tumors.
The team also tested the approach in mice prone to highly invasive tumors in their mammary glands. When the first tumor reached a certain size, the researchers injected it with CpG and anti-OX40. Both the injected and any noninjected tumors regressed. The mice were also protected against tumors arising in other mammary glands. The treatment increased the survival time of these cancer-prone mice as well.
“This is a very targeted approach,” Levy says. “Only the tumor that shares the protein targets displayed by the treated site is affected. We’re attacking specific targets without having to identify exactly what proteins the T cells are recognizing.”
Preliminary experiments in cancer patients suggested this approach could translate to human cancer. CpG and anti-OX40 are both already being studied in clinical trials. A clinical trial has now been launched to test this vaccination approach in combination with low dose local radiation in people with lymphoma.
—by Harrison Wein, Ph.D.
Related Links
- Boosting Immunotherapy Against Brain Cancer
- Personalized Immunotherapy Treats Epithelial Cancer
- Technique Directs Immune Cells to Target Leukemia
- Immunotherapy: Using the Immune System to Treat Cancer
References: Eradication of spontaneous malignancy by local immunotherapy. Sagiv-Barfi I, Czerwinski DK, Levy S, Alam IS, Mayer AT, Gambhir SS, Levy R. Sci Transl Med. 2018 Jan 31;10(426). pii: eaan4488. doi: 10.1126/scitranslmed.aan4488. PMID: 29386357.
Funding: NIH’s National Cancer Institute (NCI); Leukemia and Lymphoma Society; Boaz and Varda Dotan Foundation; and Phil N. Allen Foundation.
