You are here
October 24, 2017
Blocking stomach acid may promote chronic liver disease
At a Glance
- A new study found that blocking stomach acid can lead to an overgrowth of intestinal bacteria that likely contributes to liver inflammation and damage.
- The findings suggest that some widely used acid reflux (heartburn) medications may worsen chronic liver disease.

The liver has many important functions, including helping to digest food and process and distribute nutrients. A healthy liver is necessary for survival. The liver can regenerate after being damaged. However, repeated or long-lasting injury can cause scar tissue to form. Scarring of the liver may lead to cirrhosis, a condition in which the liver is unable to function normally. Liver cirrhosis is a leading cause of death worldwide.
Many conditions can contribute to the development of cirrhosis, including obesity, which is associated with non-alcoholic fatty liver disease (NAFLD), and non-alcoholic steatohepatitis (NASH), a form of NAFLD in which you also have inflammation and liver cell damage. But alcohol misuse accounts for about half of cirrhosis-related deaths.
Changes in your gut’s microorganisms, or microbiota, can affect the progression of liver disease. Misusing alcohol alters the microbes in your gut. So can a commonly used class of heartburn medication called proton pump inhibitors (PPIs), which block stomach acid secretion. PPIs are often used by people who have chronic liver disease. However, the impact of these medications on liver disease progression has been unknown.
To investigate whether blocking stomach acid affects chronic liver disease, a team led by Dr. Bernd Schnabl at the University of California San Diego School of Medicine looked at PPIs in mouse models of three types of liver disease—alcohol-induced liver disease, NAFLD, and NASH—and in humans. The study was funded in part by NIH’s National Institute on Alcohol Abuse and Alcoholism (NIAAA). Results were published on October 16, 2017 in Nature Communications.
The team blocked stomach acid in the mice either by genetically deleting the gene that controls stomach acid secretion or by administering the PPI omeprazole (Prilosec). Liver conditions in all three disease models were worsened when the mice lacked stomach acid.
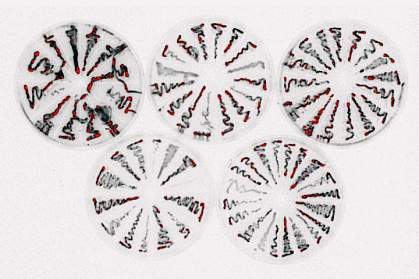
The researchers found that mice lacking stomach acid had higher levels of intestinal bacteria as well as imbalances among the microbes. In particular, the mice had increased levels of Enterococcus in their guts. Further experiments suggested that these bacteria can reach the liver, where they can cause liver inflammation and damage.
The team looked at whether people taking PPIs have similar microbiota changes. They collected fecal samples from healthy people before and after PPI treatment. After two weeks, those taking the PPI treatment also had a higher number of Enterococcus.
The researchers next investigated whether there might be a link between PPIs and the development of alcoholic liver disease. They looked at 4,830 patients with a diagnosis of alcohol use disorder. Among these, 36% had been using PPIs. The analysis showed that PPI use increased the 10-year risk of developing liver disease (20.7% for active users; 16.1% for previous users; 12.4% for those who had never used PPIs).
“Our findings indicate that the recent rise in use of [stomach] acid-suppressing medications might have contributed to the increased incidence of chronic liver disease,” Schnabl says. “We believe clinicians should consider withholding medications that suppress [stomach] acid unless there is a strong medical indication.”
—Tianna Hicklin, Ph.D.
Related Links
- Fungi in the Gut Linked to Alcoholic Liver Disease
- Diet Affects Autoinflammatory Disease Via Gut Microbes
- The Healthy Human Microbiome
- Your Liver Delivers: Protect It From Harm
- Your Microbes and You: The Good, Bad and Ugly
- Liver Disease
- Cirrhosis
- Nonalcoholic Fatty Liver Disease & NASH
- Acid Reflux (GER & GERD) in Adults
- Human Microbiome Project
References: Gastric acid suppression promotes alcoholic liver disease by inducing overgrowth of intestinal Enterococcus. Llorente C, Jepsen P, Inamine T, Wang L, Bluemel S, Wang HJ, Loomba R, Bajaj JS, Schubert ML, Sikaroodi M, Gillevet PM, Xu J, Kisseleva T, Ho SB, DePew J, Du X, Sørensen HT, Vilstrup H, Nelson KE, Brenner DA, Fouts DE, Schnabl B. Nat Commun. 2017 Oct 16;8(1):837. doi: 10.1038/s41467-017-00796-x. PMID: 29038503.
Funding: NIH’s National Institute on Alcohol Abuse and Alcoholism (NIAAA); U.S. Department of Veterans Affairs; and the Swiss National Foundation.
