You are here
August 10, 2021
Cellular defect found in inherited and sporadic ALS
At a Glance
- In lab-grown neurons derived from people with inherited or sporadic ALS, buildup of a protein called CHMP7 in the nucleus led to cellular damage.
- Using a drug to block this buildup prevented damage, suggesting a strategy to treat both inherited and sporadic ALS.
Amyotrophic lateral sclerosis, or ALS, is a rapidly progressive, fatal disease. It affects the nerve cells (neurons) in the brain and spinal cord that control voluntary muscle movements like walking, breathing, and talking. No cure has yet been found.
About 10% of cases of ALS are caused by inherited mutations. The other 90% occur sporadically, with no known genetic cause. It hasn’t been clear if the two types of disease have common drivers, and if they could potentially be treated using similar approaches.
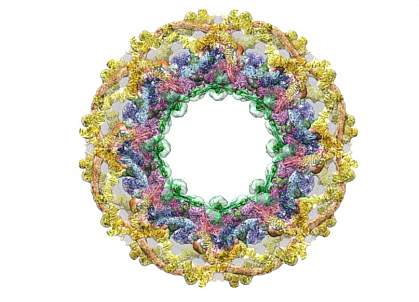
A research team led by Dr. Jeffrey Rothstein from Johns Hopkins University has been looking at the role of the nuclear pore complex in ALS and related diseases. Nuclear pores help control what goes in and out of the nucleus (where DNA resides). Changes in nuclear pores within neurons are known to occur early in one type of inherited ALS.
To understand if nuclear pore damage helps drive sporadic ALS as well, the researchers studied lab-grown neurons derived from skin or blood cells taken from people with and without the disease. They also looked at tissue samples taken from the brains of people who died of ALS.
The team first measured changes in molecules that form the nuclear pore complex, called nucleoporins. The study was funded in part by NIH’s National Institute of Neurological Disorders and Stroke (NINDS). Results were published on July 28, 2021, in Science Translational Medicine.
Neurons grown from the cells of people with either inherited or sporadic ALS had a reduction in nucleoporins in their nuclei. This could potentially destabilize nuclear pores.
Additional work showed that a protein called CHMP7 accumulated in the nuclei of cells from people with both types of ALS. CHMP7 is usually found outside the nucleus and is known to play a role in keeping nuclear pores intact. CHMP7 buildup occurred before the reduction in nucleoporins. This suggests it may play a role in nuclear pore damage. A buildup of CHMP7 in the nuclei was also found in samples taken from patients in areas of the brain known to be affected by ALS.
The accumulation of CHMP7 in nuclei caused other effects similar to those seen in people with ALS. A protein called TDP-43 normally functions in the nucleus to process the RNA molecules that carry genetic instructions to make proteins. But in people with late-stage ALS, it’s found outside the nucleus. The team showed that, when CHMP7 couldn’t be transported out of the nuclei of neurons, TDP-43 leaked out, leading to problems in RNA processing.
Using a drug to lower levels of CHMP7 in the nucleus kept nuclear pores intact in cells derived from people with either inherited or sporadic disease. The treatment also stopped TDP-43 from leaking out of the nucleus, restored gene activity, and reduced signs of stress in neurons.
“There is considerable interest in identifying new therapeutic targets for ALS, particularly for the sporadic form of the disorder,” says Dr. Amelie Gubitz, a program director at NINDS. “Gene-targeting strategies like the one shown here now allow us to move from biological discovery straight to therapy development.”
Related Links
- ALS-Related Mutations Prevent RNA Transport in Nerves
- A Biomarker for Tracking the Progression of ALS
- Dormant Viral Genes May Awaken to Cause ALS
- Treatment Shows Promise in Models of Fatal Neurological Disorders
- Nuclear Pore Problems May Lead to ALS and Dementia
- New Genetic Mutations Discovered in Families with ALS
- All About ALS: Understanding a Devastating Disorder
- Amyotrophic Lateral Sclerosis (ALS) Fact Sheet
- Amyotrophic Lateral Sclerosis (ALS) Information Page
References: Nuclear accumulation of CHMP7 initiates nuclear pore complex injury and subsequent TDP-43 dysfunction in sporadic and familial ALS. Coyne AN, Baskerville V, Zaepfel BL, Dickson DW, Rigo F, Bennett F, Lusk CP, Rothstein JD. Sci Transl Med. 2021 Jul 28;13(604):eabe1923. doi: 10.1126/scitranslmed.abe1923. PMID: 34321318.
Funding: NIH’s National Institute of Neurological Disorders and Stroke (NINDS); Department of Defense; Robert Packard Center for ALS Research; ALS Finding a Cure; ALS Association; Muscular Dystrophy Association; Virginia Gentleman Foundation; F Prime; Chan Zuckerberg Initiative.
