You are here
April 22, 2013
Cholesterol as Target for Age-Related Vision Loss
A study in mice suggests that targeting cholesterol metabolism in the eye may help prevent progression of a severe form of age-related macular degeneration (AMD), one of the most common causes of blindness in older Americans.
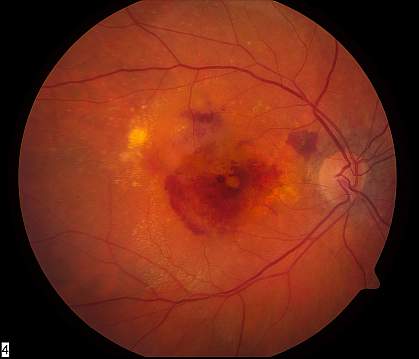
AMD involves the macula, the central portion of the retina that allows us to look straight ahead and see detailed images. In one type of advanced AMD, abnormal blood vessels grow and leak fluid and blood into the macula, obscuring central vision. Without treatment, most patients with this form of AMD — called neovascular or “wet” AMD — lose the ability to drive, read and recognize faces. Treatments are available but carry risks of complications, and there’s no cure.
The causes of neovascular AMD are unclear. One hallmark of AMD is the appearance of drusen, yellow deposits under the retina that contain cholesterol and other debris. Small drusen are a normal part of aging, but larger drusen are often found in patients with AMD. Drusen and the cholesterol within them have been prime suspects in AMD. Studies have linked cholesterol metabolism genes with AMD risk as well.
A team led by Dr. Rajendra Apte at Washington University in St. Louis suspected that macrophages, a type of immune cell, might play a role in the progression of AMD. These cells scavenge and engulf debris. In earlier work, the team found that macrophages normally help limit the growth of new blood vessels in the eye, but the cells lose this ability with age. Their further investigations were funded in part by NIH’s National Eye Institute (NEI), National Heart, Lung and Blood Institute (NHLBI) and National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK). The study appeared in Cell Metabolism on April 2, 2013.
The team examined cholesterol metabolism in macrophages from young and old mice. They found that macrophages from the older mice had lower levels of ABCA1, a protein needed for macrophages to release cholesterol into the bloodstream. They also found lower ABCA1 levels in blood cells (the source of macrophages) from older people (ages 67-87) than from younger people (ages 25-34).
The researchers then grew macrophages together with blood vessel cells. Young macrophages efficiently stopped blood vessel cells from multiplying, but old macrophages didn’t. Deleting the ABCA1 gene in young macrophages caused them to behave like old macrophages. Next, the researchers tried treating old macrophages with a drug known to enhance cholesterol transport in the cells by raising levels of ABCA1. The drug, called a liver X receptor (LXR) agonist, rejuvenated old macrophages and enabled them to inhibit growth of blood vessel cells.
Finally, the researchers tested the LXR agonist in mice with an eye injury that spurs abnormal blood vessel growth similar to that seen in neovascular AMD. Eye drops of the drug significantly reduced the blood vessel growth.
“Ideally, macrophages should take up cholesterol, process it, and spit it out into the bloodstream,” Apte says. “In AMD, we think the cells are ingesting cholesterol but not able to spit it out. So you get these inflamed macrophages that promote blood vessel growth.”
The results suggest that LXR agonists or other drugs that help macrophages clear away cholesterol might prove effective for treating AMD. Further study is needed to explore whether high blood cholesterol — and cholesterol-modifying drugs like statins — affect the disease.
Related Links
- Cholesterol Genes Tied to Age-Related Macular Degeneration
- The Genetics of Age-Related Macular Degeneration
- Age-Related Macular Degeneration
References: Cell Metab. 2013 Apr 2;17(4):549-61. doi: 10.1016/j.cmet.2013.03.009. PMID: 23562078.
Funding: NIH’s National Eye Institute (NEI), National Heart, Lung and Blood Institute (NHLBI) and National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK), along with the U.S. Civilian Research and Development Foundation, the Carl Marshall Reeves and Mildred Almen Reeves Foundation Inc., the Research to Prevent Blindness Inc., the International Retina Research Foundation, the American Health Assistance Foundation, the Lacy Foundation and the Thome Foundation.
