You are here
May 18, 2021
Delivering RNA therapies to brain tumors
At a Glance
- A combination of nanoparticle packaging and focused ultrasound allowed an RNA therapy to be delivered across the blood-brain barrier in mice.
- Brain tumors in mice treated using the combination experienced substantial cell death, suggesting its feasibility as a brain cancer therapy.
Ribonucleic acid, better known as RNA, is a workhorse molecule in the body. Different types of RNA do everything from helping produce proteins to regulating the activity (or expression) of genes.
Research into using RNA to treat diseases and disorders is expanding rapidly. RNA forms the backbone of several vaccines being used to prevent COVID-19. In the field of cancer research, scientists are interested in using RNA-based therapies to treat brain tumors, which are often resistant to standard chemotherapy and radiation therapy.
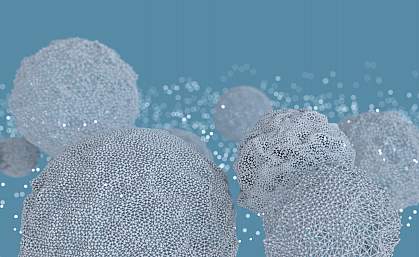
Scientists have been testing a type of RNA called small interfering RNA, or siRNA, as a brain tumor treatment. SiRNA can block the expression of genes that drive cancer growth. But RNA is fragile. To help it survive in the body long enough to have an effect, it has to be packaged in some type of microscopic carrier.
These carriers face another hurdle: they’re usually too large to get past the blood-brain barrier. The blood-brain barrier is a dense barrier of cells that prevents harmful materials in the blood from entering the brain.
To circumvent these obstacles, a research team led by Dr. Costas Arvanitis from the Georgia Institute of Technology, in collaboration with Dr. Tobey MacDonald at Emory University, used a two-pronged strategy. They packaged siRNA that can shut down certain cancer-driving genes into specialized nanoparticles. These nanoparticles were designed to protect siRNA in the bloodstream and be taken up by cancer cells.
The team then tested these nanoparticles in mice in combination with a technique called microbubble-enhanced focused ultrasound. After injection of a type of tiny gas bubble, low-intensity ultrasound beams aimed at the blood-brain barrier makes the bubbles vibrate vigorously. This briefly disrupts part of the blood-brain barrier enough to allow the nanoparticles to get through and reach the cancer cells.
The study was funded in part by NIH’s National Institute of Biomedical Imaging and Bioengineering (NIBIB) and National Cancer Institute (NCI). Results were published on April 30, 2021, in Science Advances.
In the brains of healthy mice, the ultrasound technique increased the amount of nanoparticles that passed into the brain by more than 10-fold. In mice with brain tumors, the team measured a 10-fold increase with the use of ultrasound in the amount of both siRNA and nanoparticles that got past the blood-brain barrier.
The siRNA that reached the tumors was still active and shut down a target gene. Correspondingly, the researchers saw a 16-fold increase in tumor cell death with the combination of siRNA-loaded nanoparticles plus ultrasound, compared to siRNA-loaded nanoparticles alone.
The low-intensity ultrasound beams used were well within established safety limits. However, further work will be needed to refine the treatment to optimize its effects and confirm that the technique doesn’t negatively impact brain tissue.
“This technology can provide an effective treatment with minimal side effects, which is very exciting,” Arvanitis says. “Now we are moving forward to try and identify what components are missing to translate this technology to the clinic.”
—by Sharon Reynolds
Related Links
- Nanoparticles Developed for Traumatic Brain Injury
- How Cancer Vesicles Breach the Blood-Brain Barrier
- Blood-Brain Barrier Test May Predict Dementia
- Chemotherapy Using Nanoparticles
- Can Oxygen “Microbubbles” Make Radiation Therapy More Effective?
- Ultrasound
- Inside the Cell: RNA’s Many Talents
References: Single-cell analysis reveals effective siRNA delivery in brain tumors with microbubble-enhanced ultrasound and cationic nanoparticles. Guo Y, Lee H, Fang Z, Velalopoulou A, Kim J, Thomas MB, Liu J, Abramowitz RG, Kim Y, Coskun AF, Krummel DP, Sengupta S, MacDonald TJ, Arvanitis C. Sci Adv. 2021 Apr 30;7(18):eabf7390. doi: 10.1126/sciadv.abf7390. Print 2021 Apr. PMID: 33931452.
Funding: NIH’s National Institute of Biomedical Imaging and Bioengineering (NIBIB) and National Cancer Institute (NCI); CURE Foundation; Harold C. Schott Foundation; Pam and Tom Mischell Foundation.
