You are here
April 27, 2015
Drugs Lessen Multiple Sclerosis Damage in Mice
At a Glance
- In a mouse study, 2 drugs already on the market activated stem cells and repaired the type of brain damage seen in multiple sclerosis (MS).
- More research will be needed to determine whether the drugs could lead to novel MS therapies.
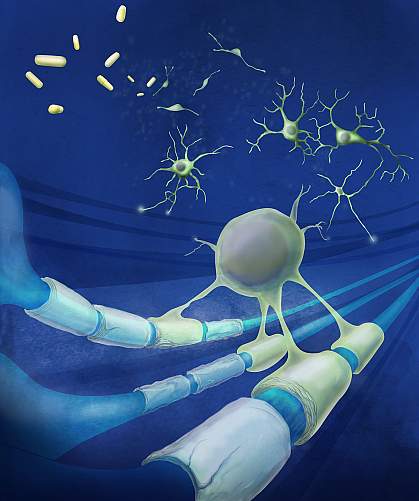
MS is a disease in which a nerve-insulating compound called myelin is mistakenly attacked by the immune system. The breakdown of myelin disrupts communication between the brain and the body, leading to muscle weakness, numbness, and problems with vision, coordination, and balance.
What triggers the disease is unknown. Anti-inflammatory drugs, which modulate the immune system, can help prevent the episodic relapses common in MS. However, they’re less effective at preventing chronic disease and disability. An alternate approach might be to develop therapies that promote myelin repair.
Myelin is laid down around nerve cells by specialized cells called oligodendrocytes in a process called myelination. Oligodendrocytes are derived from stem cells called oligodendrocyte progenitor cells (OPCs). OPCs multiply in the brains of MS patients, but for unknown reasons fail to form oligodendrocytes that can remyelinate nerve cells.
A research team led by Dr. Paul J. Tesar at Case Western Reserve University and Dr. Robert Miller at George Washington University investigated whether drugs already approved for other uses could stimulate OPCs and boost myelination. The study was partially funded by NIH’s National Institute of Neurological Disorders and Stroke (NINDS). Results appeared online inNature on April 20, 2015.
The scientists began with mouse OPCs and screened compounds for their ability to boost production of a protein that marks oligodendrocytes. They tested more than 700 drugs with a history of safe use in humans. The compounds came from a drug library maintained by NIH’s National Center for Advancing Translational Sciences (NCATS).
The researchers found that 2 compounds, miconazole (an antifungal) and clobetasol (a steroid), stimulated mouse OPCs into generating oligodendrocytes. Tests confirmed that the drugs also induced human OPCs to differentiate into oligodendrocytes.
The team next examined whether the drugs could improve remyelination when injected into a mouse model of MS. Both drugs were effective in activating OPCs to enhance myelination and reverse paralysis. Almost all of the animals regained use of their hind limbs. Further investigation showed that the drugs acted through 2 distinct molecular mechanisms.
“Our ultimate goal was to enhance the body’s ability to repair itself,” Tesar says. The researchers caution that more research is needed before these drugs can be tested to treat people with MS in clinical trials. The compounds are currently only approved for use as creams or powders on the surface of the body. Their safety when used in other forms, such as injections, is unknown.
The research team is also planning to expand the library of drugs screened against OPCs in the near future to identify other promising compounds.
Related Links
- Immune System Reset May Halt Multiple Sclerosis Progression
- Vitamin D Levels Predict Multiple Sclerosis Progression
- Landmark Analysis Probes Nature vs. Nurture in Multiple Sclerosis
- The Mystery of Multiple Sclerosis: No Simple Explanation
- Multiple Sclerosis: Hope Through Research
- Repurposing Drugs
References: Drug-based modulation of endogenous stem cells promotes functional remyelination in vivo. Najm FJ, Madhavan M, Zaremba A, Shick E, Karl RT, Factor DC, Miller TE, Nevin ZS, Kantor C, Sargent A, Quick KL, Schlatzer DM, Tang H, Papoian R, Brimacombe KR, Shen M, Boxer MB, Jadhav A, Robinson AP, Podojil JR, Miller SD, Miller RH, Tesar PJ. Nature. 2015 Apr 20. doi: 10.1038/nature14335. [Epub ahead of print]. PMID: 25896324.
Funding: NIH’s National Institute of Neurological Disorders and Stroke (NINDS), National Institute of General Medical Sciences (NIGMS), and National Cancer Institute (NCI); New York Stem Cell Foundation; Myelin Repair Foundation; Mt. Sinai Health Care Foundation; CWRU Council to Advance Human Health; the Goodman, Long, and Geller families; and New York Stem Cell Foundation.
