You are here
September 10, 2019
How brown fat improves metabolism
At a Glance
- Researchers gained key insights into brown fat’s effects on the body’s metabolism.
- The findings reveal targets for developing new treatments for obesity and diabetes.
Metabolism involves the chemical reactions that break down the food we eat into sugars, fats, and amino acids. We use these compounds for energy to power our bodies. They may also be used to build new cell structures and machinery. Metabolism can be impacted by many factors, such as diet, genes, the environment, and daily activity.
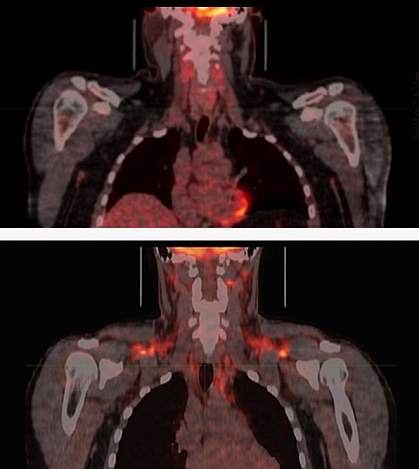
Brown fat breaks down blood sugar (glucose) and fat molecules to create heat and help maintain body temperature. Cold temperatures activate brown fat, which leads to various metabolic changes in the body. Most of our fat, however, is white fat, which stores extra energy. Too much white fat builds up in obesity. Researchers have been working to harness brown fat’s activity in order to treat obesity, diabetes, and other metabolic disorders.
To gain a deeper understanding of how brown fat affects metabolism, a team led by Dr. Shingo Kajimura at the University of California, San Francisco, carefully analyzed blood levels of glucose, fats, and amino acids before and after activation of brown fat in 33 healthy young men (average age about 23 years old). The work was funded in part by NIH’s National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK). Results were published online on August 21, 2019, in Nature.
Based on measurements taken at normal room temperature, the team classified 17 of the men as having high brown fat activity and 16 as low activity. They then exposed the men to a temperature cold enough to activate their brown fat (but not low enough to cause them to shiver) for two hours.
Unexpectedly, the team found that the men with high brown fat activity had reduced levels of compounds called branched chain amino acids (BCAAs) in their bloodstreams. This change wasn’t seen in the men with low brown fat activity. Experiments in obese mice confirmed that cold exposure reduced BCAAs in rodents with brown fat, too.
BCAAs include three essential amino acids—valine, leucine, and isoleucine—that are important for many functions in the body. For example, your muscles can use BCAAs to provide energy during exercise. However, past studies have linked high levels of BCAAs with obesity, insulin resistance, and type 2 diabetes in people and rodents.
The scientists carried out a series of experiments to further investigate the relationship between brown fat and BCAAs. They found that brown fat produces a protein called SLC25A44 upon cold exposure. SLC25A44 brings BCAAs into mitochondria, the cell’s energy compartment, where they are used to produce energy and generate heat. Blocking this process in mice led to higher BCAA levels, obesity, and signs of diabetes.
“The findings suggest that boosting SLC25A44 activity, thereby enhancing BCAA utilization, may be a promising strategy for removing excess BCAAs from the bloodstream and potentially treating conditions such as obesity and diabetes,” Kajimura says.
—by Harrison Wein, Ph.D.
Related Links
- Microneedle Patch Shrinks Fat Tissue in Mice
- Nanoparticles Target, Transform Fat Tissue
- Fat Tissue Can Communicate with Other Organs
- Insights into Energy-Burning Fat Cells
- Drug Activates Brown Fat and Increases Metabolism
- Cool Temperature Alters Human Fat and Metabolism
- Understanding Adult Overweight & Obesity
- Dietary Supplements for Exercise and Athletic Performance
References: BCAA catabolism in brown fat controls energy homeostasis through SLC25A44. Yoneshiro T, Wang Q, Tajima K, Matsushita M, Maki H, Igarashi K, Dai Z, White PJ, McGarrah RW, Ilkayeva OR, Deleye Y, Oguri Y, Kuroda M, Ikeda K, Li H, Ueno A, Ohishi M, Ishikawa T, Kim K, Chen Y, Sponton CH, Pradhan RN, Majd H, Greiner VJ, Yoneshiro M, Brown Z, Chondronikola M, Takahashi H, Goto T, Kawada T, Sidossis L, Szoka FC, McManus MT, Saito M, Soga T, Kajimura S. Nature. 2019 Aug 21. doi: 10.1038/s41586-019-1503-x. [Epub ahead of print]. PMID: 31435015.
Funding: NIH’s National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK) and National Cancer Institute (NCI); Edward Mallinckrodt Jr. Foundation; American Diabetes Association; Japan Agency for Medical Research and Development; Japan Society for the Promotion of Science.
