You are here
June 8, 2021
How COVID-19 variants evade immune response
At a Glance
- Research revealed how certain mutations in circulating SARS-CoV-2 variants allow the virus to avoid neutralization by many antibodies.
- The results suggest how to develop more broadly effective therapies and vaccines.
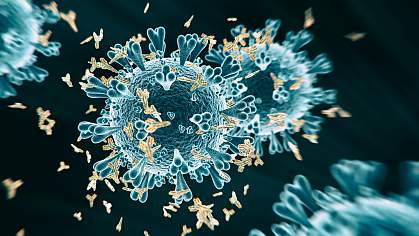
SARS-CoV-2, the virus that causes COVID-19, uses a protein called the spike protein to recognize and enter host cells. Recent SARS-CoV-2 variants contain changes, or mutations, at a key site on the spike protein called the receptor-binding site (RBS).
Some of these mutations render antibodies elicited against earlier virus strains less effective. This allows the variants to partially escape the immune response produced after vaccination or prior infection. It raises concerns that new variants could make existing vaccines less effective and draw out the pandemic.
Researchers led by Dr. Ian Wilson at the Scripps Research Institute examined how and why certain mutations protect the virus. NIH’s National Institute of Allergy and Infectious Diseases (NIAID) supported the research, which appeared in Science on May 20, 2021.
Proteins like the SARS-CoV-2 spike consist of long chains of building blocks called amino acids that fold into a specific shape. A mutation in the viral genome can lead to an amino acid getting replaced by one of a different type. This can, in turn, alter the protein’s structure and function. The variants first identified in South Africa and Brazil share mutations in three locations in the RBS: 417, 484, and 501.
The research team tested how well antibodies from COVID-19 patients bound to viruses that had these mutations. Most antibodies elicited against SARS-CoV-2 belong to two main classes. The mutations at positions 417 and 484 prevented binding by antibodies from these classes. The position 417 mutation also weakened virus binding to host cells. But the mutation at position 501 offset this effect by enhancing host cell binding.
The researchers investigated why these mutations prevent antibody binding and neutralization. They analyzed the molecular structures of more than 50 human antibodies bound to the SARS-CoV-2 spike protein. Antibodies from the two main classes almost always interact with the amino acid at position 417 or 484 when binding to the RBS. Changing either amino acid would disrupt these interactions and interfere with antibody binding.
“This work provides a structural explanation for why antibodies elicited by COVID-19 vaccines or natural infection by the original pandemic strain are often ineffective against these variants of concern,” Wilson says.
The researchers also tested antibodies that bind to parts of the spike protein outside of the RBS. These antibodies could still effectively bind and neutralize the virus even in the presence of the mutations of interest. Notably, these antibodies are effective against many related coronaviruses. Thus, vaccines and antibodies targeting sites outside of the RBS could protect against a range of virus variants. Such broad protection will be especially important if SARS-CoV-2 never gets completely eliminated.
“In designing next-generation vaccines and antibody therapies, we should consider increasing the focus on other vulnerable sites on the virus that tend not to be affected by the mutations found in variants of concern,” says co-lead author Dr. Meng Yuan.
—by Brian Doctrow, Ph.D.
Related Links
- Immune Response to Vaccination After COVID-19
- SARS-CoV-2 Antibodies Protect from Reinfection
- Experimental Coronavirus Vaccine Highly Effective
- Potent Neutralizing Antibodies Target New Regions of Coronavirus Spike
- Potent Antibodies Found in People Recovered From COVID-19
- Novel Coronavirus Structure Reveals Targets for Vaccines and Treatments
- Developing Therapeutics and Vaccines for Coronaviruses
- Coronavirus (COVID-19)
- COVID-19 (CDC)
References: Structural and functional ramifications of antigenic drift in recent SARS-CoV-2 variants. Yuan M, Huang D, Lee CD, Wu NC, Jackson AM, Zhu X, Liu H, Peng L, van Gils MJ, Sanders RW, Burton DR, Reincke SM, Prüss H, Kreye J, Nemazee D, Ward AB, Wilson IA. Science. 2021 May 20:eabh1139. doi: 10.1126/science.abh1139. Online ahead of print. PMID: 34016740.
Funding: NIH’s National Institute of Allergy and Infectious Diseases (NIAID); Bill and Melinda Gates Foundation; German Research Foundation; Helmholtz Association; German Federal Ministry of Education and Research; Netherlands Organization for Scientific Research; United States Department of Energy.
