You are here
February 12, 2019
Immune cells in the gut slow metabolism
At a Glance
- A type of immune cell found in the mouse gut slows metabolism and raises the risk of diabetes and heart disease.
- More studies are needed to see if targeting these cells in people could help reduce the risk of obesity and diseases related to diet.
The rate of metabolism—how the body breaks down food into the fuel it needs—can vary widely between people. Some people metabolize food more quickly, and others more slowly. People with slower metabolisms may be at greater risk of weight gain and resulting health conditions. The metabolic process is complex, however, and many aspects are not fully understood.
A research team led by Dr. Filip Swirski from Harvard Medical School has been studying the relationship between the immune system and metabolism. They noticed that mice lacking a protein called integrin β7 had unusually high metabolisms. Integrin β7 is known to direct immune cells to the gut. Mice lacking this protein could eat more food than mice that had it without gaining weight, despite similar levels of activity.
The researchers designed a set of experiments to understand how integrin β7 affects metabolism. They also looked at whether it influences the risk of heart disease, diabetes, and other diseases associated with diet. The project was funded in part by NIH’s National Heart, Lung, and Blood Institute (NHLBI). Results were published on January 30, 2019, in Nature.
The team found that mice lacking integrin β7 were more sensitive to insulin than mice with a normal amount of the protein. When fed a diet high in fat, sugar, and sodium, mice without integrin β7 didn't gain a substantial amount of weight, as mice that produced the protein did. Mice lacking integrin β7 also developed about half the amount of arterial plaque as regular mice in response to an unhealthy diet. Plaque buildup, or atherosclerosis, can lead to serious health problems, including heart attack and stroke.
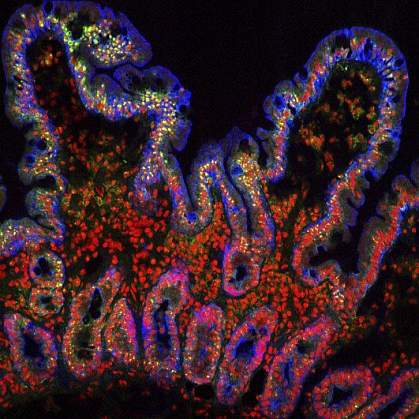
Drilling down to the cellular level, the researchers found that one class of immune cell that integrin β7 helps guide to the gut, intraepithelial T lymphocytes (IELs), appeared to be the ones driving the effects of integrin β7 on metabolism. IELs are known to help protect the body from harmful microbes in the gut.
The researchers found that IELs in the gut were hoarding a protein called GLP-1. GLP-1 encourages the body to produce insulin and controls blood sugar levels. The team found that the absence of integrin β7, which led to fewer IELs in the gut, allowed higher GLP-1 levels into the bloodstream. This ramped up metabolism and reduced the risk of diabetes and heart disease in mice.
Reducing the amount of GLP-1 in the bloodstream, and thereby slowing metabolism, may be advantageous when food is scarce. This was the case for much of human history. “Now with food so abundant, this energy-saving mechanism can backfire and lead to unhealthy outcomes,” Swirski says.
Further research is needed to better understand the metabolic role of IELs in the body. Targeting these cells in people could potentially help to treat diseases such as obesity, high cholesterol, diabetes, and high blood pressure.
Related Links
- How Night Shifts Disrupt Metabolism
- Cool Temperature Alters Human Fat and Metabolism
- Genes, Junk Food and Weight
- Gut Bacteria May Influence Metabolic Syndrome
- Metabolic Network Finds Disease Links
- Metabolic Syndrome
- Overweight and Obesity
References: Gut intraepithelial T cells calibrate metabolism and accelerate cardiovascular disease. He S, Kahles F, Rattik S, Nairz M, McAlpine CS, Anzai A, Selgrade D, Fenn AM, Chan CT, Mindur JE, Valet C, Poller WC, Halle L, Rotllan N, Iwamoto Y, Wojtkiewicz GR, Weissleder R, Libby P, Fernández-Hernando C, Drucker DJ, Nahrendorf M, Swirski FK. Nature. 2019 Jan 30. doi: 10.1038/s41586-018-0849-9. [Epub ahead of print]. PMID:30700910.
Funding: NIH’s National Heart, Lung, and Blood Institute (NHLBI) and National Institute of Allergy and Infectious Diseases (NIAID); American Heart Association; Massachusetts General Hospital Research Scholars Program; German Research Foundation; Swedish Research Council; Austrian Science Fund; Boehringer Ingelheim Fonds; Canadian Institutes of Health Research; Canada Research Chairs Program; University of Toronto; and Novo Nordisk.
