You are here
February 6, 2024
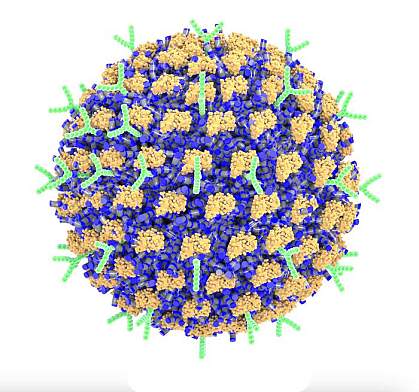
Preventing severe allergic reactions with nanoparticles
At a Glance
- Researchers created nanoparticles that could deactivate immune cells and prevent severe allergic reactions in mice.
- The findings could lead to new approaches to prevent allergies and anaphylaxis in people.
Anaphylaxis is a sudden, severe, and sometimes deadly allergic reaction. It can be triggered by exposure to certain foods, medications, or insect stings. Once a severe allergic reaction begins, it can be treated with epinephrine and other medications. But there are currently no ways to prevent anaphylactic reactions besides avoiding the triggering substances altogether.
Allergic reactions arise when the immune system reacts to a typically harmless substance, or allergen. Exposure to allergens prompts the immune system to make IgE antibodies that bind to that allergen. IgE antibodies also bind to the surfaces of immune cells known as mast cells. These cells can be activated upon later exposure to the allergen. Once activated, mast cells release histamines and other inflammatory substances. In large amounts, these substances can cause the life-threatening symptoms of anaphylaxis, such as trouble breathing and a serious drop in blood pressure.
The scientists first developed a technique to effectively coat nanoparticles with controllable amounts of both antibodies. They faced an important challenge: Antibodies are proteins, and protein structures and activities are often altered when they attach to nanoparticles. Rather than coating existing nanoparticles to link them to proteins, the researchers developed a technique to create nanoparticles composed of a small compound called poly(propylene sulfone) that allows proteins to bind without being altered.
The team coated the nanoparticles with both antibodies and confirmed that the antibody functions remained intact. Studies in human skin cells showed that nanoparticles with both types of antibodies inhibited mast cell activation. In mouse studies, intravenous injections of the nanoparticles led to near-complete prevention of anaphylaxis. No side effects were observed. In contrast, mice receiving nanoparticles without the antibodies or just given free antibodies were not protected from allergic reactions.
Lastly, to test whether the approach could prevent a reaction to a particular allergen, the team coated the nanoparticles with both an allergen and the anti-Siglec-6 antibodies. After mice were given IgE to the allergen to make them allergic, the nanoparticles proved able to protect mice against anaphylaxis caused by the allergen. This shows that the technique can be used to shut down the immune response to a specific allergen. With further development, this type of therapy holds promise for preventing allergic reactions in people.
“Currently, there are no approved drugs available to specifically target mast cells. All we have are medications like antihistamines to treat symptoms, and those don’t prevent allergies,” Scott says. “If we had a way to inactivate the mast cells that respond to specific allergens, then we could stop dangerous immune responses in severe situations like anaphylaxis, as well as less serious responses like seasonal allergies.”
The ability to create nanoparticles coated with combinations of active proteins will also enable researchers to engineer other bioactive nanoparticles for a wide range of applications.
—by Vicki Contie
Related Links
- Unexpected Role for the Nervous System in Anaphylaxis
- Nanoparticle Vaccine Against Various Coronaviruses
- Nanoparticle-Based Flu Vaccine
- Nanoparticles Developed for Traumatic Brain Injury
- Understanding Food Allergies
- Anaphylaxis
References: Controlled adsorption of multiple bioactive proteins enables targeted mast cell nanotherapy. Du F, Rische CH, Li Y, Vincent MP, Krier-Burris RA, Qian Y, Yuk SA, Almunif S, Bochner BS, Qiao B, Scott EA. Nat Nanotechnol. 2024 Jan 16. doi: 10.1038/s41565-023-01584-z. Online ahead of print. PMID: 38228804.
Funding: NIH’s National Institute of Biomedical Imaging and Bioengineering (NIBIB) and National Institute of Allergy and Infectious Diseases (NIAID).
