You are here
May 22, 2018
Squirrel hibernation tricks suggest medical uses
At a Glance
- Researchers discovered cellular mechanisms that help ground squirrels survive hibernation.
- The insights suggest ways to better preserve organs used for transplants, as well as other medical uses.
Hibernating animals like the 13-lined ground squirrel can endure near freezing temperatures that would cause severe injuries in other mammals. The cytoskeleton—the network of small structures that provides support and other crucial functions for the cell—can be particularly vulnerable to cold. Understanding how hibernating animals protect the cytoskeleton could show how to preserve human tissues kept at cold temperatures for medical uses.
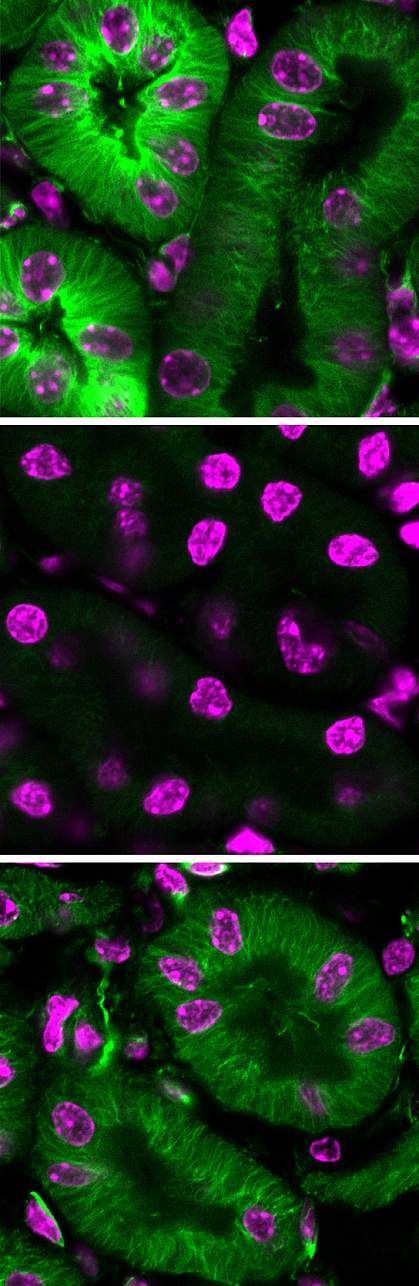
Microtubules, a major component of the cytoskeleton, quickly deteriorate in the cold. These structures are vital to many organs and the nervous system. Neurons (nerve cells) need a stable microtubule cytoskeleton to maintain their shape and connections. A team led by Drs. Wei Li and Jingxing Ou at NIH’s National Eye Institute (NEI) compared cells from non-hibernators to cells from the 13-lined ground squirrel to identify differences in their response to cold. The findings were published in the May 3, 2018, issue of Cell.
The scientists took cells from a newborn ground squirrel and genetically "reprogrammed" them to take on the characteristics of embryonic stem cells. These cells, called induced pluripotent stem cells (iPSCs), can grow indefinitely in the lab and can theoretically change into all cell types found in the body. In neurons derived from the ground squirrel iPSCs, microtubules remained intact under cold conditions.
Next, the team carefully examined the differences between iPSC-derived neurons from ground squirrels and humans. They found differences in mitochondria, the organelles that produce energy for the cell. Human mitochondria tended to overreact to the cold and produce excessive amounts of a byproduct of metabolism called reactive oxygen species (ROS). ROS can wreak havoc with microtubules. Ground squirrel ROS levels remained relatively low in cold conditions, which could help explain why their microtubules remained intact.
In the human neurons, but not in the squirrel ones, cold exposure also affected cell compartments called lysosomes. Lysosomes digest damaged proteins using enzymes called proteases. These proteases leaked from lysosomes and digested nearby microtubules in cold-exposed human neurons.
The researchers next tested two types of treatments to see whether they could protect non-hibernators against cold-induced damage: one that reduces ROS production in mitochondria and a second that inhibits proteases. After bathing human iPSC-neurons in the drugs, the scientists exposed them to cold temperatures (4oC or 39oF) for 4 to 24 hours. The drugs preserved microtubule structures. The team next tested the approach in the rat retina, the light-sensitive tissue at the back of the eye, and in mouse kidneys. The treatment protected both types of tissues at 4oC for 4 to 24 hours.
These findings pave the way for protecting human tissues during cold storage before transplantation and also during induced hypothermia following a traumatic brain injury.
“By understanding the biology of cold adaptation in hibernation, we may be able to improve and broaden the applications of induced hypothermia in the future, and perhaps prolong the viability of organs prior to transplantation,” Li says. “Kidneys, for example, are typically stored for no more than 30 hours. After that, the tissue starts to deteriorate.... Heart, lungs, and livers have an even shorter shelf life.”
Related Links
- Preserving Livers for Transplantation
- How Storing Corneas Affects Transplantation Success
- Long-Lived Pig-to-Primate Heart Transplants
- Microtubules’ Role in Heart Cell Contraction Revealed
- Organ Donation: Pass It On
References: iPSCs from a Hibernator Provide a Platform for Studying Cold Adaptation and Its Potential Medical Applications. Ou J, Ball JM, Luan Y, Zhao T, Miyagishima KJ, Xu Y, Zhou H, Chen J, Merriman DK, Xie Z, Mallon BS, Li W. Cell. 2018 May 3;173(4):851-863.e16. doi: 10.1016/j.cell.2018.03.010. Epub 2018 Mar 22. PMID: 29576452.
Funding: NIH’s National Eye Institute (NEI) and National Institute of Neurological Disorders and Stroke (NINDS); Joint Research Fund for Overseas Natural Science of China; and Center for Human Immunology, Autoimmunity, and Inflammation.
