You are here
November 21, 2023
Synthetic melanin nanoparticles for wound healing
At a Glance
- Synthetic nanoparticles made of the skin pigment melanin sped up healing of skin injuries.
- With further development, the nanoparticles could serve as a topical therapy for wound healing.
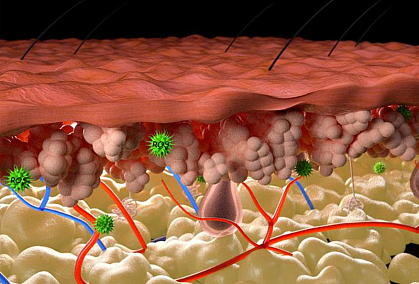
High levels of natural compounds called reactive oxygen species (ROS) can impair the healing of skin wounds. ROS are a type of molecule called radicals, which cause harmful damage to cells. Various biochemical reactions in the body produce ROS as byproducts. Examples of ROS include hydrogen peroxide, superoxides, and hydroxyl radicals.
Antioxidants protect against radicals by removing or inactivating them. One potent antioxidant is melanin, the pigment naturally found in human skin. Melanin levels in the skin increase upon exposure to ultraviolet (UV) light or harmful chemicals, both of which can create ROS.
A team of researchers led by Drs. Nathan Gianneschi and Kurt Lu at Northwestern University thought that applying melanin topically to skin injuries might aid wound healing. To test this hypothesis, they created nanoscale particles with a synthetic form of melanin. They tested the effect of these synthetic melanin particles on healing of skin wounds in mice and on human skin samples. Results appeared in npj Regenerative Medicine on November 2, 2023.
The researchers induced skin wounds in mice using either a chemical irritant or UV light. Applying the synthetic melanin particles reduced skin swelling and increased the speed at which the wound healed. Similar effects were seen in both chemically-induced and UV-induced injuries. The particles suppressed the activity of genes and signaling pathways involved in inflammation. They also boosted the activity of the antioxidant enzyme superoxide dismutase, a key part of the body’s defenses against ROS. Mice treated with the synthetic melanin had more anti-inflammatory immune cells in the skin compared with untreated mice.
“Importantly, application of the particles led to both local wound repair and a wider beneficial immune response,” Lu explains.
The team tested two types of particles: one with a high surface area and one with a low surface area. Particles with more surface area should allow for more exposure of the wound to melanin. As expected, mice treated with the high surface area particles healed faster than those treated with the low surface area ones. The high surface area particles also had a greater effect on inflammatory genes and superoxide dismutase activity.
The researchers next tested the synthetic melanin particles on human skin samples taken from people undergoing cosmetic surgery. Treatment with both types reduced the damage caused by injuries to the human skin.
These findings suggest that topical synthetic melanin could be a promising therapy to speed wound healing. Other topical antioxidants have also been shown to aid in wound healing. But the researchers note that the synthetic melanin particles have several advantages compared to other compounds.
“The synthetic melanin is capable of scavenging more radicals per gram compared to human melanin,” Gianneschi says. “It’s like super melanin. It’s biocompatible, degradable, nontoxic, and clear when rubbed onto the skin. In our studies, it acts as an efficient sponge, removing damaging factors and protecting the skin.”
—by Brian Doctrow, Ph.D.
Related Links
- Dysfunctional Exosomes Involved in Chronic Inflammation in Diabetic Wounds
- Smart Bandage Improves Wound Healing in Mice
- Poor Immune Response Impairs Diabetic Wound Healing
- Newly Identified Oral Stem Cell Key to Wound Healing
- Injected Liquid Forms a Gel in Damaged Heart
- Hydrogel-Grown Tissues Speed Wound Healing in Mouse Colon
- Blocking Scar Tissue Formation Around Medical Device Implants
- To Heal a Wound: Helping the Skin Fix Itself
- Biomaterials
- Tissue Engineering and Regenerative Medicine
References: Topical application of synthetic melanin promotes tissue repair. Biyashev D, Siwicka ZE, Onay UV, Demczuk M, Xu D, Ernst MK, Evans ST, Nguyen CV, Son FA, Paul NK, McCallum NC, Farha OK, Miller SD, Gianneschi NC, Lu KQ. NPJ Regen Med. 2023 Nov 2;8(1):61. doi: 10.1038/s41536-023-00331-1. PMID: 37919305.
Funding: NIH’s National Institute of Arthritis and Musculoskeletal and Skin Diseases (NIAMS) and National Cancer Institute (NCI); Air Force Office of Scientific Research; Defense Threat Reduction Agency; Department of Defense; International Institute for Nanotechnology.
