You are here
January 9, 2018
Technique treats hereditary deafness in mice
At a Glance
- Researchers developed a genome editing strategy to treat hearing loss in a mouse model of hereditary deafness.
- With further development, the approach might be used as a one-time treatment for certain genetic hearing loss disorders.
Some babies are born with hearing problems. Others are born with normal hearing and begin to have hearing problems as they grow older. Hearing problems in infants and children can delay the development of voice, speech, and language skills. Genetic factors are often involved in hearing loss, but options for treating genetic deafness are often limited.
A research team used a mouse model of human genetic deafness to design a potential treatment approach. The team was led by Drs. Zheng-Yi Chen and David R. Liu at Massachusetts Eye and Ear, the Broad Institute, Harvard University, and Howard Hughes Medical Institute. The work was funded in part by NIH’s National Institute on Deafness and Other Communication Disorders (NIDCD), National Institute of Biomedical Imaging and Bioengineering (NIBIB), and National Institute of General Medical Sciences (NIGMS). Results appeared in the January 11, 2018, issue of Nature.
Mutations in the TMC1 gene (transmembrane channel-like gene family 1) are known to cause hereditary deafness in both humans and mice. These mutations affect hair cells in the cochlea of the inner ear, which transform sound waves into electrical signals that the brain recognizes as sound. “Beethoven” mice have a mutation in one copy of the gene. The mutation is dominant, which means that only one mutated copy of the gene is enough to cause the disorder.
To prevent progressive hearing loss in these mice, the scientists used the CRISPR-Cas9 gene-editing system to remove this specific mutation and disable the gene. This system uses short guide RNA (sgRNA) to identify a specific genetic sequence for the Cas9 protein to cut. The scientists first tested four candidate sgRNAs in the lab to find the one most efficient at targeting the mutation.
Past CRISPR-Cas9 approaches have used harmless viruses to deliver the Cas9 gene and sgRNA into cells. Rather than insert genes, which can persist and pose safety issues, the researchers tried a different approach: to deliver complexes of the Cas9 protein and sgRNA directly into hair cells of the inner ear. They tested 17 lipids for their ability to deliver Cas9-sgRNA complexes into cells. These lipids form structures called liposomes that can encase the complexes and bring them through cell membranes and into cells.
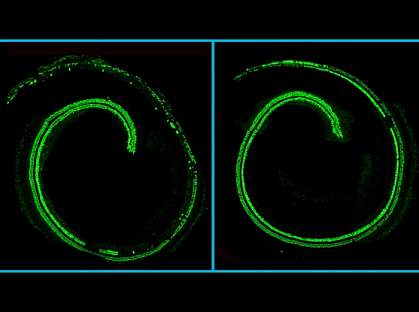
The team injected the optimal Cas9-sgRNA containing liposomes into the inner ears of neonatal mice. Eight weeks later, substantially more hair cells survived in ears that were treated. The treatment also significantly reduced progressive hearing loss. Eight weeks after treatment, treated mice startled at sounds that control mice with the genetic mutation didn’t react to.
“A lot of additional work is needed before this strategy might inform the development of a therapy for humans,” Liu says, “but at this stage, we’re delighted and excited that the treatment preserved some hearing in the animal model.”
“The strategy we used was particularly efficient in targeting dominant genetic hearing loss,” Chen says. “The therapeutic effect through local inner ear delivery also presents a major advantage in reducing potential risks.”
—by Harrison Wein, Ph.D.
Related Links
- Protein Involved in Hearing Loss Recovery
- Key Hearing Proteins Identified
- A Blueprint of Cell Development in the Inner Ear
- Hearing Different Frequencies
- How Do We Hear?
- Hearing, Ear Infections, and Deafness
- Journey of Sound to the Brain Video
References: Treatment of autosomal dominant hearing loss by in vivo delivery of genome editing agents. Gao X, Tao Y, Lamas V, Huang M, Yeh WH, Pan B, Hu YJ, Hu JH, Thompson DB, Shu Y, Li Y, Wang H, Yang S, Xu Q, Polley DB, Liberman MC, Kong WJ, Holt JR, Chen ZY, Liu DR. Nature. 2018 Jan 11;553(7687):217-221. doi: 10.1038/nature25164. Epub 2017 Dec 20. PMID: 29258297.
Funding: NIH’s National Institute on Deafness and Other Communication Disorders (NIDCD), National Institute of Biomedical Imaging and Bioengineering (NIBIB), and National Institute of General Medical Sciences (NIGMS); Defense Advanced Research Projects Agency; David-Shulsky Foundation; Frederick and Ines Yeatts Hair Cell Regeneration grant; Bertarelli Foundation; and Jeff and Kimberly Barber Fund.
