You are here
November 9, 2021
Repurposing drugs to treat age-related macular degeneration
At a Glance
- Researchers found that the antidepressant fluoxetine blocks the inflammation that leads to dry age-related macular degeneration (AMD), a common cause of vision loss.
- Health insurance data showed that people who took fluoxetine to treat depression had a reduced risk of developing dry AMD later in life.
- These results provide a rationale for clinical trials to test fluoxetine as a treatment for dry AMD.
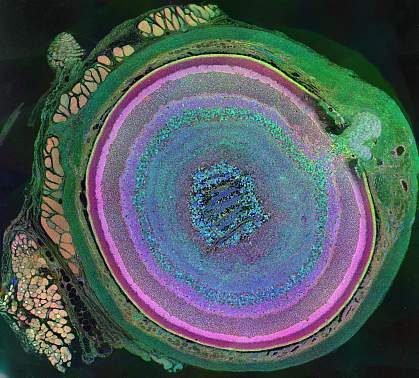
Age-related macular degeneration (AMD) is a common eye problem in older adults. It’s caused by inflammation that damages the macula, the part of the eye that controls sharp, straight-ahead vision. AMD is currently the most common cause of vision loss in adults over the age of 50 worldwide.
Most people with AMD have a type called dry AMD, also known as atrophic AMD. Treatments have been developed that can slow the progression of a less common type of AMD called wet AMD. But to date, no drugs have been approved to treat dry AMD.
Researchers led by Dr. Bradley Gelfand of the University of Virginia looked at the potential of repurposing drugs already approved for other conditions for the treatment of dry AMD.
An experimental drug called CY-09 has been found to block the inflammatory process that drives dry AMD by binding to a molecule called NLRP3. However, the testing process required to approve a new drug can take years to decades. The team looked for any drugs currently approved by the U.S. Food and Drug Administration (FDA) that are structurally and functionally similar to CY-09.
Their work was funded in part by NIH’s National Eye Institute (NEI) and National Institute of General Medical Sciences (NIGMS). Results were published on October 12, 2021, in the Proceedings of the National Academy of Sciences.
In structural studies, the researchers found that fluoxetine—an antidepressant best known by its brand name, Prozac—was similar to CY-09. Further work in the lab found that fluoxetine could bind to NLRP3 in a manner similar to CY-09.
In studies in cells, fluoxetine blocked the inflammatory cascade set off by NLRP3 that eventually leads to damage in the eye. In a mouse model of dry AMD, injections of fluoxetine into the eye protected the macula from inflammation and degeneration. In contrast, eight other antidepressants didn't block AMD progression.
Fluoxetine has been widely used to treat depression for more than three decades. To see whether the drug might alter the risk of dry AMD in people, the team analyzed health claims data from more than 100 million Americans collected between 2006 and 2018.
After accounting for other factors known to be associated with dry AMD—including age, gender, smoking, body mass index, and overall health—the researchers found that people who took fluoxetine at some point in their lives had an average 15% lower risk of developing dry AMD.
“These findings are an exciting example of the promise of drug repurposing, using existing medicines in new and unexpected ways,” Gelfand says. “Ultimately, the best way to test whether fluoxetine benefits macular degeneration is to run a prospective clinical trial.”
—by Sharon Reynolds
Related Links
- Lab-Made Eye Cells Restore Vision in Mice
- How Diet May Affect Age-Related Macular Degeneration
- Long-Term Benefits of Age-Related Macular Degeneration Treatments
- Refining Supplements for a Blinding Eye Disease
- The Genetics of Age-Related Macular Degeneration
- Age-Related Macular Degeneration
- Repurposing Drugs
References: Identification of fluoxetine as a direct NLRP3 inhibitor to treat atrophic macular degeneration. Ambati M, Apicella I, Wang SB, Narendran S, Leung H, Pereira F, Nagasaka Y, Huang P, Varshney A, Baker KL, Marion KM, Shadmehr M, Stains CI, Werner BC, Sadda SR, Taylor EW, Sutton SS, Magagnoli J, Gelfand BD. Proc Natl Acad Sci U S A. 2021 Oct 12;118(41):e2102975118. doi: 10.1073/pnas.2102975118. PMID: 34620711.
Funding: NIH’s National Eye Institute (NEI) and National Institute of General Medical Sciences (NIGMS); University of Virginia; BrightFocus Foundation; Owens Family Foundation; H2020 West-Life; European Open Science Cloud Hub.
