You are here
January 11, 2022
Experimental mRNA HIV vaccine shows promise in animals
At a Glance
- A novel HIV vaccine using mRNA technology was safe and reduced the risk of HIV-like infection in monkeys.
- The findings could be an early step in developing an effective mRNA vaccine for HIV.
Messenger RNA, or mRNA, is a molecule that tells the body how to make proteins. Vaccines based on mRNA are newly available to the public. These vaccines instruct your cells to make certain proteins from a virus or other microbe. These harmless pieces can trigger the body’s immune response. That immune response produces antibodies and cells that help protect you against getting infected if the real virus enters the body.
The first two FDA-approved COVID-19 vaccines have been extremely successful and helped launch the technology. But researchers have been studying mRNA technology for other uses for decades. Researchers are now investigating whether mRNA can be used to create vaccines that protect against other viruses.
A team led by Dr. Paolo Lusso of NIH’s National Institute of Allergy and Infectious Diseases (NIAID) developed and tested an mRNA HIV vaccine in animals. Results of the study were published in Nature Medicine on December 9, 2021.
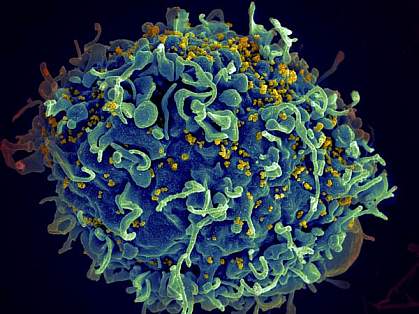
The experimental HIV vaccine is injected into muscle, where it delivers instructions for making two key HIV proteins, Env and Gag. Muscle cells assemble these two proteins into virus-like particles that are studded with many copies of Env on their surface. These virus-like particles cannot cause infection or disease because they lack the complete genetic code of HIV. Yet they provoke immune responses similar to natural HIV infection.
The researchers first tested the vaccine in mice. They found that, after two injections, it elicited antibodies in all animals that could neutralize HIV. The Env proteins on the virus-like particles produced from the vaccine closely mimicked natural infection. This represents an improvement over previous experimental HIV vaccines.
They then tested the vaccine in rhesus macaques. Monkeys received a priming vaccine followed by several booster inoculations. By week 58, all vaccinated macaques had developed measurable levels of antibodies that could neutralize many diverse HIV strains. The experimental vaccine also induced other important immune responses, like helper T cells, which aid other immune cells.
The macaques were then exposed weekly to simian-human HIV (SHIV), a form of the virus used for modeling human HIV in monkeys. After 13 weeks of virus inoculations, two out of seven immunized macaques remained uninfected. The other immunized animals had a delay in infection, which occurred after eight weeks, on average. In contrast, unimmunized animals became infected on average after three weeks. Overall, vaccinated monkeys had a 79% lower per-exposure risk of SHIV infection than unvaccinated animals.
The vaccine course was well-tolerated with only mild side effects. These results showed that the novel HIV vaccine was safe and prompted immune responses against an HIV-like virus.
“Despite nearly four decades of effort by the global research community, an effective vaccine to prevent HIV remains an elusive goal,” says Dr. Anthony Fauci, NIAID director and co-author of the study. “This experimental mRNA vaccine combines several features that may overcome shortcomings of other experimental HIV vaccines and thus represents a promising approach.”
The team plans to conduct a Phase 1 trial of the mRNA HIV vaccine in healthy adult volunteers after further refinement and testing.
Related Links
- Study Sheds Light on Key Steps in The HIV Life Cycle
- New Strategies Drive HIV from Cellular Hiding Places
- Antibody Combination Suppresses HIV
- Benefits of Early Antiretroviral Therapy in HIV Infection
- Compound May Protect Against HIV
- HIV Vaccine Progress in Animal Studies
- Key HIV Protein Structure Revealed
- HIV/AIDS
- HIV.gov
References: A multiclade env-gag VLP mRNA vaccine elicits tier-2 HIV-1-neutralizing antibodies and reduces the risk of heterologous SHIV infection in macaques. Zhang P, Narayanan E, Liu Q, Tsybovsky Y, Boswell K, Ding S, Hu Z, Follmann D, Lin Y, Miao H, Schmeisser H, Rogers D, Falcone S, Elbashir SM, Presnyak V, Bahl K, Prabhakaran M, Chen X, Sarfo EK, Ambrozak DR, Gautam R, Martin MA, Swerczek J, Herbert R, Weiss D, Misamore J, Ciaramella G, Himansu S, Stewart-Jones G, McDermott A, Koup RA, Mascola JR, Finzi A, Carfi A, Fauci AS, Lusso P. Nat Med. 2021 Dec;27(12):2234-2245. doi: 10.1038/s41591-021-01574-5. Epub 2021 Dec 9. PMID: 34887575
Funding: NIH’s National Institute of Allergy and Infectious Diseases (NIAID), National Cancer Institute (NCI), and Office of AIDS Research (OAR); Bill and Melinda Gates Foundation.
